Fracture, Cervical Spine
Introduction
Background
Approximately 5-10% of unconscious patients who present to the ED as the result of a motor vehicle accident or fall have a major injury to the cervical spine. Most cervical spine fractures occur predominantly at 2 levels. One third of injuries occur at the level of C2, and one half of injuries occur at the level of C6 or C7. Most fatal cervical spine injuries occur in upper cervical levels, either at craniocervical junction C1 or C2.
The normal anatomy of the cervical spine consists of 7 cervical vertebrae separated by intervertebral disks and joined by a complex network of ligaments. These ligaments keep individual bony elements behaving as a single unit.
View the cervical spine as 3 distinct columns: anterior, middle, and posterior. The anterior column is composed of the anterior longitudinal ligament and the anterior two thirds of the vertebral bodies, the annulus fibrosus and the intervertebral disks. The middle column is composed of the posterior longitudinal ligament and the posterior one third of the vertebral bodies, the annulus and intervertebral disks. The posterior column contains all of the bony elements formed by the pedicles, transverse processes, articulating facets, laminae, and spinous processes.
The anterior and posterior longitudinal ligaments maintain the structural integrity of the anterior and middle columns. The posterior column is held in alignment by a complex ligamentous system, including the nuchal ligament complex, capsular ligaments, and the ligamenta flava.
If one column is disrupted, other columns may provide sufficient stability to prevent spinal cord injury. If 2 columns are disrupted, the spine may move as 2 separate units, increasing the likelihood of spinal cord injury.
The atlas (C1) and the axis (C2) differ markedly from other cervical vertebrae. The atlas has no vertebral body; however, it is composed of a thick anterior arch with 2 prominent lateral masses and a thin posterior arch. The axis contains the odontoid process that represents fused remnants of the atlas body. The odontoid process is held in tight approximation to the posterior aspect of the anterior arch of C1 by the transverse ligament, which stabilizes the atlantoaxial joint.
Apical, alar, and transverse ligaments provide further stabilization by allowing spinal column rotation; this prevents posterior displacement of the dens in relation to the atlas.
For more information, see Medscape's Fracture Resource Center and Spinal Disorders Resource Center.
For more information, see Medscape's Fracture Resource Center and Spinal Disorders Resource Center.
Pathophysiology
Cervical spine injuries are best classified according to several mechanisms of injury. These include flexion, flexion-rotation, extension, extension-rotation, vertical compression, lateral flexion, and imprecisely understood mechanisms that may result in odontoid fractures and atlanto-occipital dislocation.
Flexion injury
Flexion injury
Common injuries associated with a flexion mechanism include the following:
- Simple wedge compression fracture without posterior disruption
- Flexion teardrop fracture
- Anterior subluxation
- Bilateral facet dislocation
- Clay shoveler fracture
- Anterior atlantoaxial dislocation
Simple wedge fracture
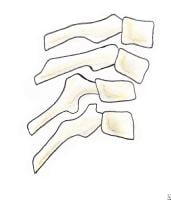
With a pure flexion injury, a longitudinal pull is exerted on the nuchal ligament complex that, because of its strength, usually remains intact. The anterior vertebral body bears most of the force, sustaining simple wedge compression anteriorly without any posterior disruption.
Radiographically the anterior border of the vertebral body has diminished height and increased concavity along with increased density due to bony impaction (see Image 2A). The prevertebral soft tissues are swollen.
(A) Simple wedge fracture with a flexion mechanism of injury is stable. (B) Flexion teardrop fracture with a flexion mechanism is unstable.
The posterior column remains intact, making this a stable fracture that requires only use of a cervical orthosis for treatment.
Flexion teardrop fracture
A flexion teardrop fracture occurs when flexion of the spine, along with vertical axial compression, causes a fracture of the anteroinferior aspect of the vertebral body. This fragment is displaced anteriorly and resembles a teardrop (see Image 2B). For this fragment to be produced significant posterior ligamentous disruption must occur. Since the fragment displaces anteriorly, a significant degree of anterior ligamentous disruption exists.
This injury involves disruption of all 3 columns, making this an extremely unstable fracture that frequently is associated with spinal cord injury. Initial management is application of traction with cervical tongs.
Anterior subluxation
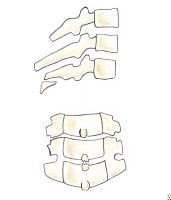
Anterior subluxation in the cervical spine occurs when posterior ligamentous complexes (nuchal ligament, capsular ligaments, ligamenta flava, posterior longitudinal ligament) rupture. The anterior longitudinal ligament remains intact. No associated bony injury is seen.
Radiographically, the lateral view shows widening of interspinous processes, and anterior and posterior contour lines are disrupted in flexion views (see Image 3). Since the anterior columns remain intact, this fracture is considered mechanically stable by definition.
Anterior subluxation with a flexion mechanism is stable in extension but potentially unstable in flexion.
Anterior subluxation is rarely associated with neurologic sequelae. Nevertheless, most authorities approach this injury as if it were potentially unstable because of the significant displacement that can occur with flexion, and very rare cases have associated neurologic deficit.
Bilateral facet dislocation
Bilateral facet dislocation is an extreme form of anterior subluxation that occurs when a significant degree of flexion and anterior subluxation causes ligamentous disruption to extend anteriorly, which causes significant anterior displacement of the spine at the level of injury. This injury involves the annulus fibrosus, anterior longitudinal ligament and posterior ligamentous complex. At the level of injury, ie, the upper vertebrae, inferior articulating facets pass superior and anterior to the superior articulating facets of the lower involved vertebrae because of extreme flexion of the spine.
Radiographically, this is seen as a displacement of more than half of the anteroposterior diameter of the vertebral body in the lateral view (see Image 4).
Bilateral facet dislocation with a flexion mechanism is extremely unstable and can have an associated disk herniation that impinges on the spinal cord during reduction.
This is an extremely unstable condition and is associated with a high prevalence of spinal cord injuries. Initial management is closed reduction and traction with cervical tongs. A significant number of bilateral facet dislocations are accompanied by disk herniation. In patients with these injuries further neurologic damage may occur if the injured disk retropulses into the canal during the application of cervical traction. Therefore, a careful neurologic examination should accompany closed reduction in these patients.
Clay shoveler fracture
Abrupt flexion of the neck, combined with a heavy upper body and lower neck muscular contraction, results in an oblique fracture of the base of the spinous process, which is avulsed by the intact and powerful supraspinous ligament. Fracture also occurs with direct blows to the spinous process or with trauma to the occiput that causes forced flexion of the neck.
Injury commonly is observed in a lateral view, since the avulsed fragment is readily evident (see Image 5A). Injury commonly occurs in lower cervical vertebrae; therefore, visualization of the C7-T1 junction in the lateral view is imperative. Injury also may be seen in the anteroposterior view as a vertically split appearance of the spinous process in the lower vertebrae (see Image 5B).
Clay shoveler fracture. (A) Lateral view of this fracture caused by a flexion mechanism shows that it is stable and represents an avulsion fracture of the base of the spinous process near the supraspinous ligament. (B) Anteroposterior view shows the vertically split appearance of the spinous process.
Since injury involves only the spinous process, this fracture is considered stable, and it is not associated with neurologic impairment. Management involves only cervical immobilization with an orthotic device for comfort.
Flexion-rotation injury
Common injuries associated with a flexion-rotation mechanism include unilateral facet dislocation and rotary atlantoaxial dislocation.
Unilateral facet dislocation
Unilateral facet dislocation occurs when flexion, along with rotation, forces one inferior articular facet of an upper vertebra to pass superior and anterior to the superior articular facet of a lower vertebra, coming to rest in the intervertebral foramen (see Image 6A). Although the posterior ligament is disrupted, vertebrae are locked in place, making this injury stable.
Radiographically, the lateral view shows an anterior displacement of the spine at the involved level of less than one half the diameter of the vertebral body. This is in contrast to the greater displacement seen with a bilateral facet dislocation, as discussed above. The anteroposterior view is useful in diagnosis of unilateral dislocation because it shows a disruption in the line connecting the spinous processes at the level of the dislocation (see Image 6B). The oblique view is also useful because it shows a disruption of the typical shingles appearance at the level of the involved vertebra (see Image 6C). The dislocated superior articulating facet of the lower vertebra is seen projecting within the neural foramina.
Unilateral facet dislocation. (A) Lateral view of this fracture caused by a flexion-rotation mechanism shows that it is stable. Anterior displacement of spine is less than one half of the diameter of a vertebral body. (B) Anteroposterior view shows disruption of a line connecting spinous processes at the level of the dislocation. (C) Oblique view shows that the expected tiling of the laminae is disrupted, and the dislocated superior articulating facet of the lower vertebra is seen projecting within the neural foramina.
The injury seldom is associated with neurologic deficits. The orthopedic consultant performs initial management, applying cervical traction to attempt closed reduction.
Rotary atlantoaxial dislocation
This injury is a specific type of unilateral facet dislocation.
Radiographically, the odontoid view shows asymmetry of the lateral masses of C1 with respect to the dens along with unilateral magnification of a lateral mass of C1 (wink sign). However, since the atlantoaxial joint permits flexion, extension, rotation, and lateral bending, radiographic asymmetry is produced when the head is tilted laterally or rotated or if a slightly oblique odontoid view is obtained despite perfect head positioning. To confirm true dislocation, basilar skull structures (jugular foramina) should appear symmetric in the presence of the findings described above.
This injury is considered unstable because of its location.
Extension injury
Common injuries associated with an extension mechanism include hangman fracture, extension teardrop fracture, fracture of the posterior arch of C1 (posterior neural arch fracture of C1) and posterior atlantoaxial dislocation.
Hangman fracture (traumatic spondylolisthesis of C2)
The name of this injury is derived from the typical fracture that occurs after hangings. Presently, it commonly is caused by motor vehicle collisions and entails bilateral fractures through the pedicles of C2 due to hyperextension.
Radiographically, a fracture line should be evident extending through the pedicles of C2 along with obvious disruption of the spinolaminar contour line (see Image 7).
Hangman fracture caused by an extension mechanism is unstable. Fracture line is evident in the lateral projection extending through pedicles of C2, along with disruption of the spinolaminar line. Sometimes, this fracture is associated with unilateral or bilateral facet dislocation, which makes it highly unstable.
Although considered an unstable fracture, it seldom is associated with spinal injury, since the anteroposterior diameter of the spinal canal is greatest at this level, and the fractured pedicles allow decompression. When associated with unilateral or bilateral facet dislocation at the level of C2, this particular type of hangman fracture is unstable and has a high rate of neurologic complications that require immediate referral for cervical traction to reduce the facet dislocation. All other types of hangman fracture can be managed initially with a cervical orthotic device.
Extension teardrop fracture
As with flexion teardrop fracture, extension teardrop fracture also manifests with a displaced anteroinferior bony fragment. This fracture occurs when the anterior longitudinal ligament pulls fragment away from the inferior aspect of the vertebra because of sudden hyperextension. The fragment is a true avulsion, in contrast to the flexion teardrop fracture in which the fragment is produced by compression of the anterior vertebral aspect due to hyperflexion.
The fracture is common after diving accidents and tends to occur at lower cervical levels. It also may be associated with the central cord syndrome due to buckling of the ligamenta flava into spinal canal during the hyperextension phase of injury.
This injury is stable in flexion but highly unstable in extension. Initial management is avoidance of iatrogenic extension and cervical traction with tongs.
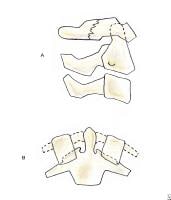
Fracture of the posterior arch of C1 fracture (posterior neural arch fracture)
This fracture occurs when the head is hyperextended and the posterior neural arch of C1 is compressed between the occiput and the strong, prominent spinous process of C2, causing the weak posterior arch of C1 to fracture (see Image 8A).
(A) Fracture of the posterior arch of C1 fracture caused by an extension mechanism is stable. Lateral projection shows a fracture line through the posterior neural arch without widening predental space. An odontoid view must be obtained to differentiate this benign fracture from a Jefferson fracture. (B) Jefferson fracture caused by a vertical (axial) compression mechanism is unstable. This fracture of all aspects of the C1 ring is associated with possible disruption of the transverse ligament of the atlas. Lateral projection may show a widened predental space and a fracture through the posterior arch of C1. Odontoid view shows displacement of the lateral masses of C1, allowing distinction of this fracture from a simple fracture of the posterior neural arch of C1.
Radiographically, the lateral projection shows a fracture line through the posterior neural arch. The odontoid view fails to show any displacement of the lateral masses of C1 with respect to the articular pillars of C2, a finding that distinguishes this fracture from a Jefferson fracture.
The transverse ligament and the anterior arch of C1 are not involved, making this fracture stable. Initial management involves the differentiation of this benign fracture from a Jefferson fracture. Once this is accomplished, only use of a cervical orthosis is required.
Vertical (axial) compression injury
Common injuries associated with a vertical compression mechanism include Jefferson fracture (burst fracture of the ring of C1), burst fracture (dispersion, axial loading), atlas fracture, and isolated fracture of the lateral mass of C1 (pillar fracture).
Jefferson fracture (burst fracture of the ring of C1)
This fracture is caused by a compressive downward force that is transmitted evenly through the occipital condyles to the superior articular surfaces of the lateral masses of C1. The process displaces the masses laterally and causes fractures of the anterior and posterior arches, along with possible disruption of the transverse ligament. Quadruple fracture of all 4 aspects of the C1 ring occurs.
Radiographically the fracture is characterized by bilateral lateral displacement of the articular masses of C1. The odontoid view shows unilateral or bilateral displacement of the lateral masses of C1 with respect to the articular pillars of C2; this finding differentiates it from a simple fracture of the posterior neural arch of C1 (see Image 8B). The lateral projection usually reveals a striking amount of prevertebral soft tissue edema.
When displacement of the lateral masses is more than 6.9 mm complete disruption of the transverse ligament has occurred and immediate referral for cervical traction is warranted. If displacement is less than 6.9 mm, the transverse ligament is still competent and neurologic injury is unlikely.
Burst fracture of the vertebral body
When downward compressive force is transmitted to lower levels in the cervical spine, the body of the cervical vertebra can shatter outward, causing a burst fracture. This fracture involves disruption of the anterior and middle columns, with a variable degree of posterior protrusion of the latter.
Radiographically, this fracture is evidenced by a vertical fracture line in the frontal projection and by comminution and protrusion of the vertebral body anteriorly and posteriorly with respect to the contiguous vertebrae in the lateral view (see Image 9). Posterior protrusion of the middle column may extend into the spinal canal and can be associated with anterior cord syndrome. Burst fractures always require an axial CT scan or MRI to document amount of middle column retropulsion.
Burst fracture of vertebral body caused by a vertical (axial) compression mechanism is stable mechanically and involves disruption of the anterior and middle columns, with variable degree of protrusion of the latter. This middle column posterior protrusion may extend into the spinal canal and be associated with an anterior cord syndrome.
Initial management of burst fractures with a loss in height of more than 25%, retropulsion, or neurologic deficit is accomplished by applying traction with cervical tongs. When none of those problems exist, the fracture is considered stable.
Multiple or complex injuries
Common injuries associated with multiple or complex mechanisms include odontoid fracture, fracture of the transverse process of C2 (lateral flexion), atlanto-occipital dislocation (flexion or extension with a shearing component), and occipital condyle fracture (vertical compression with lateral bending).
Mechanism of injury, location, and clinical relevance
Upper cervical spine (occiput to C2) injuries
Injuries at the upper cervical level are considered unstable because of their location. Nevertheless, since the diameter of the spinal canal is greatest at the level of C2, spinal cord injury from compression is the exception rather than the rule. Incompletely understood mechanisms or a combination of mechanisms usually produce injuries encountered at this level.
Common injuries include fracture of the atlas, atlantoaxial subluxation, odontoid fracture, and hangman fracture (see Extension injury above). Less common injuries include occipital condyle fracture, atlanto-occipital dislocation, atlantoaxial rotary subluxation (see Flexion-rotation injury above), and C2 lateral mass fracture.
Atlas (C1) fractures
Four types of atlas fractures (I, II, III, IV) result from impaction of the occipital condyles on the atlas, causing single or multiple fractures around the ring.
The first 2 types of atlas fracture are stable and include isolated fractures of the anterior and posterior arch of C1 (posterior arch fracture is described under Extension injury). Anterior arch fractures usually are avulsion fractures from the anterior portion of the ring and have a low morbidity rate and little clinical significance. The third type of atlas fracture is a fracture through the lateral mass of C1. Radiographically, asymmetric displacement of the mass from the rest of the vertebra is seen in the odontoid view. This fracture also has a low morbidity rate and little clinical significance.
The fourth type of atlas fracture is the burst fracture of the ring of C1 and also is known as a Jefferson fracture (discussed under Vertical (axial) compression injury above). This is the most significant type of atlas fracture from a clinical standpoint because it is associated with neurologic impairment.
The fourth type of atlas fracture is the burst fracture of the ring of C1 and also is known as a Jefferson fracture (discussed under Vertical (axial) compression injury above). This is the most significant type of atlas fracture from a clinical standpoint because it is associated with neurologic impairment.
Initial management of types I, II, and III atlas fractures consists of placement of a cervical orthosis. Type IV fracture, or Jefferson fracture, is managed with cervical traction.
Atlantoaxial subluxation
When flexion occurs without a lateral or rotatory component at the upper cervical level, it can cause an anterior dislocation at the atlantoaxial joint if the transverse ligament is disrupted. Because this joint is near the skull, shearing forces also play a part in the mechanism causing this injury, as the skull grinds the C1-C2 complex in flexion. Since the transverse ligament is the main stabilizing force of the atlantoaxial joint, this injury is unstable. Neurologic injury may occur from cord compression between the odontoid and posterior arch of C1.
Radiographically, this injury is suspected if the predental space is more than 3.5 mm (5 mm in children); axial CT is used to confirm the diagnosis. These injuries may require fusion of C1 and C2 for definitive management.
Atlanto-occipital dislocation
When severe flexion or extension exists at the upper cervical level, atlanto-occipital dislocation may occur. Atlanto-occipital dislocation involves complete disruption of all ligamentous relationships between the occiput and the atlas. Death usually occurs immediately from stretching of the brainstem, which causes respiratory arrest.
Radiographically, disassociation between the base of the occiput and the arch of C1 is seen. Cervical traction is absolutely contraindicated, since further stretching of the brainstem can occur.
Odontoid process fractures
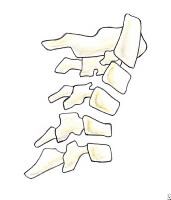
The 3 types of odontoid process fractures are classified based on the anatomic level at which the fracture occurs (see Image 1).
Odontoid fractures. (A) Type I odontoid fracture represents an avulsion of the tip of the dens at the insertion site of the alar ligament. Although mechanically stable, it is associated with life-threatening atlanto-occipital dislocation. (B) Type II odontoid fracture is a fracture at the base of the dens. This is the most common type of odontoid fracture. (C) With type III odontoid fracture, the fracture line extends into the body of the axis.
- Type I odontoid fracture is an avulsion of the tip of the dens at the insertion site of the alar ligament. Although a type I fracture is mechanically stable, it often is seen in association with atlanto-occipital dislocation and must be ruled out because of this potentially life-threatening complication.
- Type II fractures occur at the base of the dens and are the most common odontoid fractures. This type is associated with a high prevalence of nonunion due to the limited vascular supply and small area of cancellous bone.
- Type III odontoid fracture occurs when the fracture line extends into the body of the axis. Nonunion is not a major problem with these injuries because of a good blood supply and the greater amount of cancellous bone.
With types II and III fractures, the fractured segment may be displaced anteriorly, laterally, or posteriorly. Since posterior displacement of segment is more common, the prevalence of spinal cord injury is as high as 10% with these fractures.
Initial management of a type I dens fracture is use of a cervical orthosis. Manage types II and III fractures by applying traction with cervical tongs.
Occipital condyle fracture
Occipital condyle fractures are caused by a combination of vertical compression and lateral bending. Avulsion of the condylar process or a comminuted compression fracture may occur secondary to this mechanism. These fractures are associated with significant head trauma and usually are accompanied by cranial nerve deficits.
Radiographically, they are difficult to delineate, and axial CT may be required to identify them.
These mechanically stable injuries require only orthotic immobilization for management, and most heal uneventfully. These fractures are significant because of the injuries that usually accompany them.
Mechanical instability
Column disruption may lead to mechanical instability of the cervical spine. The degree of instability depends on several factors that may translate into neurologic disability, secondary to spinal cord compression. A full spectrum of cervical injuries with varying degrees of clinical importance, from the clinically insignificant to the potentially disastrous, exists. As many as 39% of cervical fractures have some degree of associated neurologic deficit.
The risk of neurologic injury, secondary to spinal injury, increases with degenerative changes related to aging, arthritic conditions (rheumatoid arthritis, ankylosing spondylitis), spinal stenosis, spina bifida, and os odontoideum, as well as the specific mechanism and location of the injury.
Trafton has ranked specific cervical injuries based on their degree of mechanical instability.1 The list below ranks cervical spine injuries in order of instability (most to least unstable):
- Rupture of the transverse ligament of the atlas
- Fracture of the dens (odontoid fracture)
- Burst fracture with posterior ligamentous disruption (flexion teardrop fracture)
- Bilateral facet dislocation
- Burst fracture without posterior ligamentous disruption
- Hyperextension fracture dislocation
- Hangman fracture
- Extension teardrop (stable in flexion)
- Jefferson fracture (burst fracture of the ring of C1)
- Unilateral facet dislocation
- Anterior subluxation
- Simple wedge compression fracture without posterior disruption
- Pillar fracture
- Fracture of the posterior arch of C1
- Spinous process fracture (clay shoveler fracture)
Frequency
United States
Cervical spine injuries cause an estimated 6000 deaths and 5000 new cases of quadriplegia each year.
Sex
Male-to-female ratio is 4:1.
Age
- Most patients with a cervical spine injury are in their prime and leading an active lifestyle prior to injury.
- Approximately 80% of patients are aged 18-25 years.
Clinical
History
Common presentations of cervical spine fracture include the following:
- Posterior neck pain on palpation of spinous processes
- Limited range of motion associated with pain
- Weakness, numbness, or paresthesias along affected nerve roots
Physical
Clinical evaluation of the cervical spine in a patient with blunt trauma is unreliable. In a study of surgical residents' ability to predict cervical injuries on the basis of clinical examination alone, sensitivity and specificity were 46% and 94%, respectively. Because of these limitations and potential for catastrophic morbidity if injury is missed, most patients with complex blunt trauma seen in the ED undergo radiographic evaluation before clearance, with some exceptions.
Common findings on physical examination in cervical spine injury include the following:
- Spinal shock
- Flaccidity
- Areflexia
- Loss of anal sphincter tone
- Fecal incontinence
- Priapism
- Loss of bulbocavernosus reflex
- Neurogenic shock
- Hypotension
- Paradoxical bradycardia
- Flushed, dry, and warm peripheral skin
- Autonomic dysfunction
- Ileus
- Urinary retention
- Poikilothermia
Causes
Motor vehicle collisions and falls account for 50% and 20% of cervical spine injuries, respectively. Recent studies have shown that the impact velocity at the time of a motor vehicle collision2,3 and airbag deployment on unrestrained drivers4,5 significantly increase the likelihood of a cervical spine injury.
Sports-related activities account for 15%. The remaining injuries are attributed to interpersonal violence. The following athletic activities have the highest incidence of associated cervical spine injuries. Participants in these events should be considered at high risk.
Sports-related activities account for 15%. The remaining injuries are attributed to interpersonal violence. The following athletic activities have the highest incidence of associated cervical spine injuries. Participants in these events should be considered at high risk.
- Diving
- Equestrian activities
- Football
- Gymnastics
- Skiing
- Hang gliding
Penetrating trauma rarely causes cervical spine fractures but may result in significant neurologic deficits.6
Cervical vertebrae
From Wikipedia, the free encyclopedia
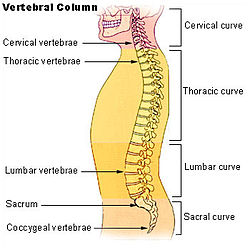
| Bone: cervical vertebrae | |
|---|---|
| Vertebral column | |
| A cervical vertebra | |
| Latin | vertebrae cervicales |
| Gray's | subject #21 97 |
| MeSH | Cervical+vertebrae |
In vertebrates, cervical vertebrae (singular: vertebra) are those vertebrae immediately inferior to the skull.
Contents[hide] |
[edit]Variation among species
In some species, some parts of the skull may be composed of vertebra-like elements, e.g. the occipital bone in humans is composed of four vertebra-like segments.
In many vertebrate species, cervical vertebrae are variable in number; however, almost allmammals have seven (including those with very short necks relative to body size, such aselephants or whales, and those with very long necks, such as giraffes). The few exceptions include the manatee and the sloths, of which the two-toed sloth has six cervical vertebrae and the three-toed sloth has up to nine cervical vertebrae (Wetzel, 1985).
In many species, though not in mammals, the cervical vertebrae bear ribs. In many other groups, such as lizards and saurischian dinosaurs, the cervical ribs are large; in birds they are small and completely fused to the vertebrae. The transverse processes of mammals are homologous to the cervical ribs of other amniotes.
Thoracic vertebrae in all species are defined as those vertebrae which also carry a pair of ribs, and lie caudal to the cervical vertebrae.
In humans, cervical vertebrae are the smallest of the true vertebrae, and can be readily distinguished from those of the thoracic or lumbarregions by the presence of a foramen (hole) in each transverse process, through which passes the vertebral artery.
The remainder of this article focuses upon human anatomy.
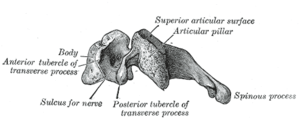
[edit]General characteristics (C3-C6)
These are the general characteristics of the third through sixth cervical vertebrae. (The first, second, and seventh vertebrae are extraordinary, and detailed later.)
- The body of these four vertebrae is small, and broader from side to side than from front to back.
- The anterior and posterior surfaces are flattened and of equal depth; the former is placed on a lower level than the latter, and its inferior border is prolonged downward, so as to overlap the upper and forepart of the vertebra below.
- The upper surface is concave transversely, and presents a projecting lip on either side;
- the lower surface is concave from front to back, convex from side to side, and presents laterally shallow concavities which receive the corresponding projecting lips of the underlying vertebra.
- The pedicles are directed laterally and backward, and are attached to the body midway between its upper and lower borders, so that the superior vertebral notch is as deep as the inferior, but it is, at the same time, narrower.
- The laminae are narrow, and thinner above than below; the vertebral foramen is large, and of a triangular form.
- The spinous process is short and bifid, the two divisions being often of unequal size.
- The superior and inferior articular processes of cervical vertebrae have fused on either or both sides to form articular pillars, columns of bone which project laterally from the junction of the pedicle and lamina.
- The articular facets are flat and of an oval form:
- the superior face backward, upward, and slightly medially.
- the inferior face forward, downward, and slightly laterally.
- The transverse processes are each pierced by the foramen transversarium, which, in the upper six vertebrae, gives passage to thevertebral artery and vein, as well as a plexus of sympathetic nerves. Each process consists of an anterior and a posterior part. These two parts are joined, outside the foramen, by a bar of bone which exhibits a deep sulcus on its upper surface for the passage of the corresponding spinal nerve.
- The anterior portion is the homologue of the rib in the thoracic region, and is therefore named the costal process or costal element. It arises from the side of the body, is directed laterally in front of the foramen, and ends in a tubercle, the anterior tubercle.
- The posterior part, the true transverse process, springs from the vertebral arch behind the foramen, and is directed forward and laterally; it ends in a flattened vertical tubercle, the posterior tubercle.
[edit]Special cervical vertebrae (C1, C2, and C7)
- C1 or atlas: The Atlas is the topmost vertebra, and – along with C2 – forms the joint connecting the skull and spine. Its chief peculiarity is that it has no body, and this is due to the fact that the body of the atlas has fused with that of the next vertebra.
- C2 or axis: It forms the pivot upon which C1 rotates. The most distinctive characteristic of this bone is the strong odontoid process (dens) which rises perpendicularly from the upper surface of the body. The body is deeper in front than behind, and prolonged downward anteriorly so as to overlap the upper and front part of the third vertebra.
- C7 or vertebra prominens: The most distinctive characteristic of this vertebra is the existence of a long and prominent spinous process, hence the name vertebra prominens. In some subjects, the seventh cervical vertebra is associated with an abnormal pair of ribs, known ascervical ribs. These ribs are usually small, but may occasionally compress blood vessels (such as the subclavian artery) or nerves in thebrachial plexus, causing ischemic muscle pain, numbness, tingling, and weakness in the upper limb.
[edit]Movements of the cervical spine
The movement of nodding the head takes place predominantly through flexion and extension at the joint between the atlas and the occipital bone, the atlanto-occipital joint. However, the cervical spine is comparatively mobile, and some component of this movement is due to flexion and extension of the vertebral column itself.
The movement of shaking or rotating the head left and right happens almost entirely at the joint between the atlas and the axis, the atlanto-axial joint. A small amount of rotation of the vertebral column itself contributes to the movement.
[edit]Landmarks
Base of Nose and the Hard palate corresponds to C1.
Teeth (when mouth remains closed) correspond to C2.
Mandible and Hyoid bone correspond to C3.
The thyroid cartilage is from C4 to C5.[1]
The cricoid cartilage is from C6 to C7.[1]
[edit]Clinical significance
Injuries to the cervical spine are common at the level of the second cervical vertebrae, but neurological injury is uncommon.
If it does occur, however, it may cause death or profound disability, including paralysis of the arms, legs, and diaphragm, which leads torespiratory failure.
Common patterns of injury include the odontoid fracture and the hangman's fracture, both of which are often treated with immobilization in acervical collar or Halo brace.
A common EMS practice is to immobilize a patient's cervical spine to prevent further damage during transport to Medical Aid. This practice has come under review recently as incidence rates of unstable spinal trauma can be as low as 2% in immobilized patients. Canadian studies have developed the Canadian C-Spine Rule (CCR) for physicians to decide who should receive radiological imaging. [2]
[edit]Additional images
Cervical Spine Anatomy (Neck)
The cervical spine begins at the base of the skull. Seven vertebrae make up the cervical spine with eight pairs of cervical nerves. The individual cervical vertebrae are abbreviated C1, C2, C3, C4, C5, C6 and C7. The cervical nerves are also abbreviated; C1 through C8.

Cervical Vertebrae and Supporting Structures
The cervical bones - the vertebrae - are smaller in size when compared to other spinal vertebrae. The purpose of the cervical spine is to contain and protect the spinal cord, support the skull, and enable diverse head movement (e.g., rotate side to side, bend forward and backward).
The cervical bones - the vertebrae - are smaller in size when compared to other spinal vertebrae. The purpose of the cervical spine is to contain and protect the spinal cord, support the skull, and enable diverse head movement (e.g., rotate side to side, bend forward and backward).
A complex system of ligaments, tendons, and muscles help to support and stabilize the cervical spine. Ligaments work to prevent excessive movement that could result in serious injury. Muscles also help to provide spinal balance and stability, and enable movement. Muscles contract and relax in response to nerve impulses originating in the brain. Some muscles work in pairs or as antagonists. This means when a muscle contracts, the opposing muscle relaxes. There are different types of muscle: forward flexors, lateral flexors, rotators, and extensors.
Spinal Cord and Cervical Nerve Roots
Nerve impulses travel to and from the brain through the spinal cord to a specific location by way of the peripheral nervous system (PNS). The PNS is the complex system of nerves that branch off from the spinal nerve roots. These nerves travel outside of the spinal canal or spinal cord into the organs, arms, legs, fingers - throughout the entire body.
Nerve impulses travel to and from the brain through the spinal cord to a specific location by way of the peripheral nervous system (PNS). The PNS is the complex system of nerves that branch off from the spinal nerve roots. These nerves travel outside of the spinal canal or spinal cord into the organs, arms, legs, fingers - throughout the entire body.
Injury or mild trauma to the cervical spine can cause a serious or life-threatening medical emergency (e.g. spinal cord injury or SCI, fracture). Pain, numbness, weakness, and tingling are symptoms that may develop when one or more spinal nerves are injured, irritated, or stretched. The cervical nerves control many bodily functions and sensory activities.
C1: Head and neck
C2: Head and neck
C3: Diaphragm
C4: Upper body muscles (e.g. Deltoids, Biceps)
C5: Wrist extensors
C6: Wrist extensors
C7: Triceps
C8: Hands
Anatomical Planes of the Body
Medical professionals often refer to sections of the body in terms of anatomical planes (flat surfaces). These planes are imaginary lines – vertical or horizontal – drawn through an upright body. The terms are used to describe a specific body part.

Listed below are general anatomical terms and their meanings.
| Anatomical Planes | |
|---|---|
| Coronal Plane or Frontal Plane | |
| Sagittal Plane or Lateral Plane | |
| Axial Plane or Transverse Plane | |
| Anatomical Terms | Direction |
| Medial | Toward the midline of the body |
| Lateral | Away from the midline of the body |
| Proximal | Toward a reference point (extremity) |
| Distal | Away from a reference point (extremity) |
| Inferior | Lower or below |
| Superior | Upper or above |
| Cephalad or Cranial | Head |
| Caudal or Caudad | Tail, tail end |
| Anterior | Toward the front |
| Posterior | Toward the back |
| Dorsal | Posterior |
| Ventral | Anterior |
Spinal Curves
n the womb and for a period of time following birth, a baby’s spine is shaped like the letter C. This curve is termed a primary curve, which is Kyphotic. During the time the baby is learning to lift his head and eventually walk, muscles develop. As muscular strength and ability is gained, the baby’s activity will shift body weight to the spine. Gradually secondary curves develop in the cervical and lumbar regions; Lordotic curves. These curves will continue to develop until growing stops.
Spinal curves are either kyphotic or lordotic. In a normal spine there are four types of spinal curvatures important to balance, flexibility, and stress absorption and distribution.
Spinal curves are either kyphotic or lordotic. In a normal spine there are four types of spinal curvatures important to balance, flexibility, and stress absorption and distribution.
 |
| Type of Spinal Curves | Curve Description |
|---|---|
| Kyphosis or Kyphotic Curve | Concave anteriorly and convex posteriorly |
| Lordosis or Lordotic Curve | Convex anteriorly and concave posteriorly |
| Curvature | Normal Curvature |
| Cervical Lordosis | 20 to 40 degrees |
| Thoracic Kyphosis | 20 to 40 degrees |
| Lumbar Lordosis | 40 to 60 degrees |
| Sacral Kyphosis | Sacrum fused in a kyphotic curve |
Vertebral Column
he spinal column (or vertebral column) extends from the skull to the pelvis and is made up of 33 individual bones termed vertebrae. The vertebrae are stacked on top of each other group into four regions:

| Term | # of Vertebrae | Body Area | Abbreviation |
|---|---|---|---|
| Cervical | 7 | Neck | C1 – C7 |
| Thoracic | 12 | Chest | T1 – T12 |
| Lumbar | 5 or 6 | Low Back | L1 – L5 |
| Sacrum | 5 (fused) | Pelvis | S1 – S5 |
| Coccyx | 3 | Tailbone | None |
Cervical Vertebrae (C1 – C7)
The cervical spine is further divided into two parts; the upper cervical region (C1 and C2), and the lower cervical region (C3 through C7). C1 is termed the Atlas and C2 the Axis. The Occiput (CO), also known as the Occipital Bone, is a flat bone that forms the back of the head.
Atlas (C1)
The Atlas is the first cervical vertebra and therefore abbreviated C1. This vertebra supports the skull. Its appearance is different from the other spinal vertebrae. The atlas is a ring of bone made up of two lateral masses joined at the front and back by the anterior arch and the posterior arch.

Axis (C2)
The Axis is the second cervical vertebra or C2. It is a blunt tooth–like process that projects upward. It is also referred to as the ‘dens’ (Latin for ‘tooth’) or odontoid process. The dens provides a type of pivot and collar allowing the head and atlas to rotate around the dens.
Thoracic Vertebrae (T1 – T12)
The thoracic vertebrae increase in size from T1 through T12. They are characterized by small pedicles, long spinous processes, and relatively large intervertebral foramen (neural passageways), which result in less incidence of nerve compression.
The Axis is the second cervical vertebra or C2. It is a blunt tooth–like process that projects upward. It is also referred to as the ‘dens’ (Latin for ‘tooth’) or odontoid process. The dens provides a type of pivot and collar allowing the head and atlas to rotate around the dens.
Thoracic Vertebrae (T1 – T12)
The thoracic vertebrae increase in size from T1 through T12. They are characterized by small pedicles, long spinous processes, and relatively large intervertebral foramen (neural passageways), which result in less incidence of nerve compression.

1-Vertebral Body 2-Spinous Process 3-Transverse Facet
4-Pedicle 5-Foramen 6-Lamina 7-Superior Facet
4-Pedicle 5-Foramen 6-Lamina 7-Superior Facet
The rib cage is joined to the thoracic vertebrae. At T11 and T12, the ribs do not attach and are so are called "floating ribs." The thoracic spine's range of motion is limited due to the many rib/vertebrae connections and the long spinous processes.

Lumbar Vertebrae (L1 – L5)
The lumbar vertebrae graduate in size from L1 through L5. These vertebrae bear much of the body's weight and related biomechanical stress. The pedicles are longer and wider than those in the thoracic spine. The spinous processes are horizontal and more squared in shape. The intervertebral foramen (neural passageways) are relatively large but nerve root compression is more common than in the thoracic spine.
The lumbar vertebrae graduate in size from L1 through L5. These vertebrae bear much of the body's weight and related biomechanical stress. The pedicles are longer and wider than those in the thoracic spine. The spinous processes are horizontal and more squared in shape. The intervertebral foramen (neural passageways) are relatively large but nerve root compression is more common than in the thoracic spine.

Purpose of the Vertebrae Although vertebrae range in size; cervical the smallest, lumbar the largest, vertebral bodies are the weight bearing structures of the spinal column. Upper body weight is distributed through the spine to the sacrum and pelvis. The natural curves in the spine, kyphotic and lordotic, provide resistance and elasticity in distributing body weight and axial loads sustained during movement.
The vertebrae are composed of many elements that are critical to the overall function of the spine, which include the intervertebral discs and facet joints.
Functions of the Vertebral or Spinal Column Include:
The vertebrae are composed of many elements that are critical to the overall function of the spine, which include the intervertebral discs and facet joints.
Functions of the Vertebral or Spinal Column Include:
| Protection |
|
| Base for Attachment |
|
| Structural Support |
|
| Flexibility and Mobility |
|
| Other |
|
Sacral Spine
The Sacrum is located behind the pelvis. Five bones (abbreviated S1 through S5) fused into a triangular shape, form the sacrum. The sacrum fits between the two hipbones connecting the spine to the pelvis. The last lumbar vertebra (L5) articulates (moves) with the sacrum. Immediately below the sacrum are five additional bones, fused together to form the Coccyx (tailbone).
The Sacrum is located behind the pelvis. Five bones (abbreviated S1 through S5) fused into a triangular shape, form the sacrum. The sacrum fits between the two hipbones connecting the spine to the pelvis. The last lumbar vertebra (L5) articulates (moves) with the sacrum. Immediately below the sacrum are five additional bones, fused together to form the Coccyx (tailbone).
Intervertebral Discs
The intervertebral discs make up one fourth of the spinal column's length. There are no discs between the Atlas (C1), Axis (C2), and Coccyx. Discs are not vascular and therefore depend on the end plates to diffuse needed nutrients. The cartilaginous layers of the end plates anchor the discs in place.
 |
The intervertebral discs are fibrocartilaginous cushions serving as the spine's shock absorbing system, which protect the vertebrae, brain, and other structures (i.e. nerves). The discs allow some vertebral motion: extension and flexion. Individual disc movement is very limited – however considerable motion is possible when several discs combine forces.
Annulus Fibrosus and Nucleus Pulposus
Intervertebral discs are composed of an annulus fibrosus and a nucleus pulposus.
Annulus Fibrosus and Nucleus Pulposus
Intervertebral discs are composed of an annulus fibrosus and a nucleus pulposus.
 |
The annulus fibrosus is a strong radial tire–like structure made up of lamellae; concentric sheets of collagen fibers connected to the vertebral end plates. The sheets are orientated at various angles. The annulus fibrosus encloses the nucleus pulposus.
Although both the annulus fibrosus and nucleus pulposus are composed of water, collagen, and proteoglycans (PGs), the amount of fluid (water and PGs) is greatest in the nucleus pulposus. PG molecules are important because they attract and retain water. The nucleus pulposus contains a hydrated gel–like matter that resists compression. The amount of water in the nucleus varies throughout the day depending on activity.
Although both the annulus fibrosus and nucleus pulposus are composed of water, collagen, and proteoglycans (PGs), the amount of fluid (water and PGs) is greatest in the nucleus pulposus. PG molecules are important because they attract and retain water. The nucleus pulposus contains a hydrated gel–like matter that resists compression. The amount of water in the nucleus varies throughout the day depending on activity.
Nerve Structures of the Spine
Nerves control the body’s functions including the vital organs, sensation, and movement. The nervous system receives information and initiates an appropriate response. It is affected by internal and external factors (ie, stimulus).
Nerves follow tracts and cross over junctions called synapses. Simplified, it is a complex communicative process between nerves conducted by chemical and/or electrical changes.
Nerves follow tracts and cross over junctions called synapses. Simplified, it is a complex communicative process between nerves conducted by chemical and/or electrical changes.
Watch our video explaining spinal anatomy—it'll give you the big picture of how the nerves and vertebrae fit together in your spine.
 |
 |
Central Nervous System (CNS)The Central Nervous System is composed of the brain and spinal cord. The brain has 12 cranial nerves. The spinal cord, which originates immediately below the brain stem, extends to the first lumbar vertebra (L1). Beyond L1 the spinal cord becomes the cauda equina (see below). The spinal cord provides a means of communication between the brain and peripheral nerves.
| BRAIN | 12 Cranial Nerves |
|---|---|
| Motor: | 5 nerves |
| Sensory: | 3 Nerves |
| Motor/Sensory: | 4 nerves |
| SPINAL CORD | 31 Pairs – Spinal Nerves |
|---|---|
| Cervical | 8 pair |
| Thoracic | 12 pair |
| Lumbar | 5 pair |
| Sacral | 5 pair |
| Coccyx | 1 pair |
Peripheral Nervous System (PNS)The CNS extends to the Peripheral Nervous System, a system of nerves that branch beyond the spinal cord, brain, and brainstem. The PNS carries information to and from the CNS.
The PNS includes the Somatic Nervous System (SNS) and the Autonomic Nervous System (ANS). The somatic nervous system includes the nerves serving the musculoskeletal system and the skin. It is voluntary and reacts to outside stimuli affecting the body. The autonomic nervous system is involuntary automatically seeking to maintain homeostasis or normal function.
The ANS is further divided into the Sympathetic Nervous System and theParasympathetic Nervous System. The sympathetic nervous system is an involuntary system often associated with the flight or fight response. The parasympathetic nervous system is responsible for promoting internal harmony such as regular heartbeat during normal activity.
Just below the last thoracic (T12) and first lumbar (L1) vertebra the spinal cord ends at the Conus Medullaris. From this point the spinal nerves, resembling a horse’s tail become known as the cauda equina extending to the coccyx. These nerves are suspended in spinal fluid.
The PNS includes the Somatic Nervous System (SNS) and the Autonomic Nervous System (ANS). The somatic nervous system includes the nerves serving the musculoskeletal system and the skin. It is voluntary and reacts to outside stimuli affecting the body. The autonomic nervous system is involuntary automatically seeking to maintain homeostasis or normal function.
The ANS is further divided into the Sympathetic Nervous System and theParasympathetic Nervous System. The sympathetic nervous system is an involuntary system often associated with the flight or fight response. The parasympathetic nervous system is responsible for promoting internal harmony such as regular heartbeat during normal activity.
Just below the last thoracic (T12) and first lumbar (L1) vertebra the spinal cord ends at the Conus Medullaris. From this point the spinal nerves, resembling a horse’s tail become known as the cauda equina extending to the coccyx. These nerves are suspended in spinal fluid.
 |
The nerve roots pass out of the spinal canal through the intervertebral foramen, where they feed the body either anteriorly (motor) or posteriorly (sensory). The anterior divisions supply the front of the spine including the limbs. The posterior divisions are distributed to the muscles behind the spine.
 |
| Spinal Nerves | |
|---|---|
| Motor |
|
| Sensory |
|
Other Spinal Cord and Nerve Structures
Cerebrospinal Fluid (CSF)
Cerebrospinal fluid is a clear fluid found in the brain chambers (Ventricles), spinal canal, and spinal cord. This fluid is secreted from the Choroids Plexus, a vascular part in the ventricles of the brain. CSF bathes and circulates among these tissues and acts as a shock absorber to protect against injury. The fluid contains different electrolytes, proteins, and glucose. In an average adult the total volume of CSF is about 150 milliliters.
Meninges
Meninges are membranes that cover and protect the brain and spinal cord. There are three primary types: (1) Dura Mater, (2) Arachnoid Mater, and (3) Pia Mater.
Cerebrospinal Fluid (CSF)
Cerebrospinal fluid is a clear fluid found in the brain chambers (Ventricles), spinal canal, and spinal cord. This fluid is secreted from the Choroids Plexus, a vascular part in the ventricles of the brain. CSF bathes and circulates among these tissues and acts as a shock absorber to protect against injury. The fluid contains different electrolytes, proteins, and glucose. In an average adult the total volume of CSF is about 150 milliliters.
Meninges
Meninges are membranes that cover and protect the brain and spinal cord. There are three primary types: (1) Dura Mater, (2) Arachnoid Mater, and (3) Pia Mater.
- The dura mater, or dura, is the gray outer layer of the spinal cord and nerve roots. It is made of strong connective tissue.
- The arachnoid mater resembles a loosely woven fabric of arteries and veins. This layer is thinner than the dura mater. The Subarachnoid space is filled with cerebrospinal fluid.
- The pia mater is the innermost layer and is a delicate and highly vascular membrane providing blood to the neural structures.
Dermatomes
A dermatome is an area of skin supplied by fibers from a single spinal nerve root.
A dermatome is an area of skin supplied by fibers from a single spinal nerve root.
Facet Joints of the Spine Anatomy
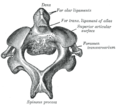
A joint is where two or more bones are joined. Joints allow motion (articulation). The joints in the spine are commonly called Facet Joints. Other names for these joints are Zygapophyseal or Apophyseal Joints.
Each vertebra has two sets of facet joints. One pair faces upward (superior articular facet) and one downward (inferior articular facet). There is one joint on each side (right and left). Facet joints are hinge–like and link vertebrae together. They are located at the back of the spine (posterior).
Each vertebra has two sets of facet joints. One pair faces upward (superior articular facet) and one downward (inferior articular facet). There is one joint on each side (right and left). Facet joints are hinge–like and link vertebrae together. They are located at the back of the spine (posterior).
 |
Facet joints are synovial joints. This means each joint is surrounded by a capsule of connective tissue and produces a fluid to nourish and lubricate the joint. The joint surfaces are coated with cartilage allowing joints to move or glide smoothly (articulate) against each other.
 |
These joints allow flexion (bend forward), extension (bend backward), and twisting motion. Certain types of movement are restricted. The spine is made more stable due to the interlocking nature to adjacent vertebrae.
Ligaments
Ligaments are fibrous bands or sheets of connective tissue linking two or more bones, cartilages, or structures together. One or more ligaments provide stability to a joint during rest and movement. Excessive movements such as hyper–extension or hyper–flexion, may be restricted by ligaments. Further, some ligaments prevent movement in certain directions.
Three of the more important ligaments in the spine are the Ligamentum Flavum, Anterior Longitudinal Ligament and the Posterior Longitudinal Ligament.
- The Ligamentum Flavum forms a cover over the dura mater: a layer of tissue that protects the spinal cord. This ligament connects under the facet joints to create a small curtain over the posterior openings between the vertebrae.
- The Anterior Longitudinal Ligament attaches to the front (anterior) of each vertebra. This ligament runs up and down the spine (vertical or longitudinal).
- The Posterior Longitudinal Ligament runs up and down behind (posterior) the spine and inside the spinal canal.

Primary Spinal Ligaments Include:
| Ligament | Spinal Region | Limits… |
|---|---|---|
| Alar | Axis – skull | Head rotation & lateral flexion |
| Anterior Atlantoaxial | Axis & Atlas | Extension |
| Posterior Atlantoaxial | Axis & Atlas | Flexion |
| Ligamentum Nuchae | Cervical | Flexion |
| Anterior Longitudinal | Axis – Sacrum | Extension & reinforces front of annulus fibrosis |
| Posterior Longitudinal | Axis – Sacrum | Flexion & reinforces back of annulus fibrosis |
| Ligamentum Flavum | Axis – Sacrum | Flexion |
| Supraspinous | Thoracic & Lumbar | Flexion |
| Interspinous | Lumbar | Flexion |
| Intertransverse | Lumbar | Lateral flexion |
| Iliolumbar | Sacroiliac joints | Stability & some motion |
| Sacroiliac | Sacroiliac joints | Stability & some motion |
| Sacrospinous | Sacroiliac joints | Stability & some motion |
| Sacrotuberous | Sacroiliac joints | Stability & some motion |

| Ligaments of the Back of the Cervical and Upper Thoracic Spine 1. Supraspinous Ligament (flexion) 2. Ligamentum Nuchae (fibrous membrane) |
Ligament Systems – Atlas and Axis
As mentioned in the Vertebral Column, the Atlas (C1) and Axis (C2) are different from the other spinal vertebrae. The upper cervical ligament system is especially important in stabilizing the upper cervical spine from the skull to C2. Although the cervical vertebrae are the smallest, the neck has the greatest range of motion.
Occipitoatlantal Ligament Complex (Atlas)
These four ligaments run between the Occiput and the Atlas:
As mentioned in the Vertebral Column, the Atlas (C1) and Axis (C2) are different from the other spinal vertebrae. The upper cervical ligament system is especially important in stabilizing the upper cervical spine from the skull to C2. Although the cervical vertebrae are the smallest, the neck has the greatest range of motion.
Occipitoatlantal Ligament Complex (Atlas)
These four ligaments run between the Occiput and the Atlas:
- Anterior Occipitoatlantal Ligament
- Posterior Occipitoatlantal Ligament
- Lateral Occipitoatlantal Ligaments (2)
Occipitoaxial Ligament Complex (Axis)These four ligaments connect the Occiput to the Axis:
- Occipitoaxial Ligament
- Alar Ligaments (2)
- Apical Ligament
Altantoaxial Ligament Complex (Axis)
These four ligaments extend from the Atlas to the Axis:
These four ligaments extend from the Atlas to the Axis:
- Anterior Atlantoaxial Ligament
- Posterior Atlantoaxial Ligament
- Lateral Ligaments (2)
Cruciate Ligament ComplexThese ligaments help to stabilize the Atlantoaxial (Axis) complex:
- Transverse Ligaments
- Superior Longitudinal Fascicles
- Inferior Longitudinal Fascicles
Spinal Muscles
Muscles are named according to their shape, location, or a combination. They are further categorized according function such as flexion, extension, or rotation. Muscles and ligaments work together to support the spine, hold it upright, and control movement during rest and activity.
| Types of Vertebral Muscles | General Location |
|---|---|
| Forward flexors | Anterior |
| Lateral flexors | Lateral |
| Rotators | Lateral |
| Extensors | Posterior |
Skeletal muscle is striated (striped) in appearance. It is innervated, under voluntary control, and has the fastest contraction rate of all muscle. Prior to a muscle contracting, a nerve impulse originates in the brain and travels through the spinal cord to the muscle.
Energy is needed for the muscle to contract (work). Mitochondria (cellular level) produce ATP (adenosine triphosphate), a chemical cells need for energy. ATP is produced as the mitochondria burn glucose (sugar). Blood vessels deliver the oxygen and nutrients the mitochondria needs to provide a steady supply of ATP.
Energy is needed for the muscle to contract (work). Mitochondria (cellular level) produce ATP (adenosine triphosphate), a chemical cells need for energy. ATP is produced as the mitochondria burn glucose (sugar). Blood vessels deliver the oxygen and nutrients the mitochondria needs to provide a steady supply of ATP.

| Muscles of the Posterior Cervical and Upper Thoracic Spine 1. Semispinalis Capitus (head rotation/pulls backward) 2. Iliocostalis Cervicis (extends cervical vertebrae) 3. Longissimus Cervicus (extends cervical vertebrae) 4. Longissimus Capitus (head rotation/pulls backward) 5. Longissimus Thoracis (extension/lateral flexion vertebral column, rib rotation) 6. Iliocostalis Thoracis (extension/lateral flexion vertebral column, rib rotation) 7. Semispinalis Thoracis (extends/rotates vertebral column) |
Muscles of the Spinal Column
| CERVICAL MUSCLES | FUNCTION | NERVE |
|---|---|---|
| Sternocleidomastoid | Extends & rotates head, flexes vertebral column | C2, C3 |
| Scalenus | Flexes & rotates neck | Lower cervical |
| Spinalis Cervicis | Extends & rotates head | Middle/lower cervical |
| Spinalis Capitus | Extends & rotates head | Middle/lower cervical |
| Semispinalis Cervicis | Extends & rotates vertebral column | Middle/lower cervical |
| Semispinalis Capitus | Rotates head & pulls backward | C1 – C5 |
| Splenius Cervicis | Extends vertebral column | Middle/lower cervical |
| Longus Colli Cervicis | Flexes cervical vertebrae | C2 – C7 |
| Longus Capitus | Flexes head | C1 – C3 |
| Rectus Capitus Anterior | Flexes head | C2, C3 |
| Rectus Capitus Lateralis | Bends head laterally | C2, C3 |
| Iliocostalis Cervicis | Extends cervical vertebrae | Middle/lower cervical |
| Longissimus Cervicis | Extends cervical vertebrae | Middle/lower cervical |
| Longissimus Capitus | Rotates head & pulls backward | Middle/lower cervical |
| Rectus Capitus Posterior Major | Extends & rotates head | Suboccipital |
| Rectus Capitus Posterior Minor | Extends head | Suboccipital |
| Obliquus Capitus Inferior | Rotates atlas | Suboccipital |
| Obliquus Capitus Superior | Extends & bends head laterally | Suboccipital |
| THORACIC MUSCLES | FUNCTION | NERVE |
|---|---|---|
| Longissimus Thoracis | Extension, lateral flexion of vertebral column, rib rotation | Dorsal primary divisions of spinal nerves |
| Iliocostalis Thoracis | Extension, lateral flexion of vertebral column, rib rotation | Dorsal primary divisions of spinal nerves |
| Spinalis Thoracis | Extends vertebral column | Dorsal primary divisions of spinal nerves |
| Semispinalis Thoracis | Extends & rotates vertebral column | Dorsal primary divisions of spinal nerves |
| Rotatores Thoracis | Extends & rotates vertebral column | Dorsal primary divisions of spinal nerves |
| LUMBAR MUSCLES | FUNCTION | NERVE |
|---|---|---|
| Psoas Major | Flexes thigh at hip joint & vertebral column | L2, L3, sometimes L1 or L4 |
| Intertransversarii Lateralis | Lateral flexion of vertebral column | Ventral primary division of spinal nerves |
| Quadratus Lumborum | Lateral flexion of vertebral column | T12, L1 |
| Interspinales | Extends vertebral column | Dorsal primary divisions of spinal nerves |
| Intertransversarii Mediales | Lateral flexion of vertebral column | Dorsal primary divisions of spinal nerves |
| Multifidus | Extends & rotates vertebral column | Dorsal primary divisions of spinal nerves |
| Longissimus Lumborum | Extends & rotates vertebral column | Dorsal primary divisions of spinal nerves |
| Iliocostalis Lumborum | Extension, lateral flexion of vertebral column, rib rotation | Dorsal primary divisions of spinal nerves |
Muscle FasciaFascia is thickened connective tissue that envelops a muscle or a group of muscles. Superficial fascia is found directly under the skin. Epimysium is the fascia closest to the muscle. Perimysium divides the muscle into facicles – muscle fibers. Endomysium is another type of connective tissue that covers each muscle fiber.
Spinal Blood Supply
The function of the vascular system is to nourish each cell in the body. This includes the vertebral column, spinal cord, neural elements, muscles, and other related structures.
Blood and Its Importance
Blood contains plasma (fluid), red blood cells (erythrocytes), white bloods cells, and platelets.
Plasma – Cell Nourishment
Plasma, the liquid part of blood, makes up 90% of blood and contains water, salts, hormones, and proteins. It delivers proteins, fats, minerals, and lipids to every cell in the body. Cells cannot reproduce or repair damage without nutrient replenishment.
Blood and Its Importance
Blood contains plasma (fluid), red blood cells (erythrocytes), white bloods cells, and platelets.
Plasma – Cell Nourishment
Plasma, the liquid part of blood, makes up 90% of blood and contains water, salts, hormones, and proteins. It delivers proteins, fats, minerals, and lipids to every cell in the body. Cells cannot reproduce or repair damage without nutrient replenishment.
 | Red = Artery Blue = Vein 1 Carotid Artery 2 Aortic Arch 3 Thoracic Aorta 4 Abdominal Aorta 5 Iliac Artery 6 Internal Jugular Vein 7 Superior Vena Cava 8 Inferior Vena Cava 9 Iliac Vein |
Oxygen – Red Blood Cells
One of the primary benefits cells derive from blood is oxygen. Cells need oxygen to burn glucose for energy. This oxygen comes from the red blood cells. Oxygenated blood is pumped from the heart via arteries and deoxygenated blood returns to the heart via veins. The Pulmonary Artery is an exception. It carries deoxygenated blood from the heart to the lungs where it is reoxygenated. The Pulmonary Vein then carries the oxygenated blood back to the heart from the lungs. The oxygenated blood is then circulated throughout the body.
Immunity – White Blood Cells
White cells are the primary components of the immune system and fight against infection and bacterial toxins. There are many types of white blood cells; neutrophils, eosinophils, lymphocytes, basophils, and monocytes – each playing a different role. Further, antibodies are transported via the circulatory system.
Clotting – Platelets
Platelets control bleeding from injury by creating a clot, or plug through a series of chemical reactions.
The spinal column is served by the body’s elaborate system of arteries and veins, as outlined in the following tables.
Arteries Supplying Spinal Column
| Arteries | Region |
|---|---|
| Vertebral | Cervical (Head) |
| Basilar | Basilar Cervical (Head) |
| Carotid | Cervical/Thoracic |
| Thoracic Aorta | Thoracic cavity |
| Intercostal | Thoracic wall |
| Spinal Branch | Thoracic/Lumbar |
| Anterior Spinal | Thoracic/Lumbar |
| Abdominal Aorta | Thoracic/Lumbar cavities |
| Posterior Branch | Thoracic to Sacrum |
| Lumbar Segmental | Lumbar |
| Left Common Iliac | Lumbar/pelvic organs, legs |
| Right Common Iliac | Lumbar/pelvic organs, legs |
| Segmental | Lumbar to Sacrum |
| Middle Sacral | Lumbosacral |
| Iliolumbar | Lumbosacral |
| Internal Iliac | Lumbosacral |
Circle of Willis
The Vertebral and Internal Carotid Arteries provide blood to the brain. These arteries give off branches that form a circle in the region of the pituitary gland. If the other two arteries are blocked, the blood vessels in the Circle of Willis provide an alternate way to feed blood to the brain.
Veins Supplying Spinal Column
The Vertebral and Internal Carotid Arteries provide blood to the brain. These arteries give off branches that form a circle in the region of the pituitary gland. If the other two arteries are blocked, the blood vessels in the Circle of Willis provide an alternate way to feed blood to the brain.
Veins Supplying Spinal Column
| Veins | Region/Comment |
|---|---|
| Internal Jugular | Cervical – returns blood from the head |
| External Jugular | Cervical – returns blood from the head |
| Superior Vena Cava | Cervical/Upper Thoracic Returns blood from upper body to heart |
| Thoracic Segmental | Thoracic |
| Inferior Vena Cava | Thoracic/Lumbosacral Returns blood from lower body to heart |
| Azygous | Lumbar – Returns blood from lower body when inferior vena cava obstructed |
| Hemiazygous | Lumbar |
| Lumbar Segmental | Lumbar |
| Left Common Iliac | Lumbar |
| Right Common Iliac | Lumbar |
| Batson’s Plexus | Lumbar – Valveless vein, provides alternate route for blood return to heart |
| Common Iliac | Lumbosacral |
Arterial Branches of the Spine
| Artery | Spinal Region | Source – Branch From |
|---|---|---|
| Anterior Radicular | Meninges Spinal Cord | Vertebral Posterior Intercostal Lumbar Lateral Sacral |
| Anterior Spinal | Meninges Spinal Cord | Vertebral Posterior Intercostal Lumbar Lateral Sacral |
| Aortic Arch | Entire Body Except Heart | Ascending Aorta |
| Basilar | Cranial Nerves Cerebellum | Vertebral |
| Brachiocephalic Trunk | Right side of head, neck, upper limb, chest wall | Aortic Arch |
| Cerebral Arterial Circle | Brain – Midbrain | Posterior Cerebral Anterior Cerebral |
| Common Carotid | Head – upper neck | Brachiocephalic Trunk Aortic Arch |
| External Carotid | Upper neck | Common Carotid |
| Great Anterior Radicular | Lower Spinal Cord | Lower Posterior Intercostal |
| Internal Carotid | Brain | Common Carotid |
| Lateral Sacral | Sacrum Sacral Nerve Roots Meninges | Internal Iliac |
| Lumbar | Spinal Cord Vertebral Column | Abdominal Aorta |
| Median Sacral | Sacrum | Abdominal Aorta |
| Middle Meningeal | Dura Mater | Maxillary |
| Posterior Radicular | Meninges, Spinal Cord | Vertebral Posterior Intercostal Lumbar Lateral Sacral |
| Posterior Spinal | Spinal Cord | Posterior Inferior Cerebellar Vertebral Posterior Intercostal Lumbar Lateral Sacral |
| Subclavian | Neck Brain Spinal Cord | Brachiocephalic Aortic Arch |
| Vertebral | Spinal Cord Neck | Subclavian |
Venous Branches of the Spine
| Vein | Spinal Region | Source(s) |
|---|---|---|
| Anterior Jugular | Neck | Submental |
| Azygos | Chest Wall | Lumbar Subcosta Posterior Intercostal |
| Brachiocephalic | Head Neck Upper Limbs | Subclavian Internal Jugular Vertebra |
| Cavernous Sinus | Brain | Superior Ophthalmic Middle Cerebral |
| External Jugular | Head Neck | Posterior Auricular Posterior External Jugular Transverse Cervical Anterior Jugular |
| External Vertebral Plexus | Vertebral Column Vertebral Muscles | Internal Vertebral Plexus |
| Hemiazygos | Lower Chest Wall | Lumbar Subcostal |
| Internal Vertebral Plexus | Spinal Cord Meninges Vertebral Column | External Vertebral Plexus |
| Posterior Intercostal | Spinal Cord Vertebra Ribs | Spinal Tributary Posterior Tributary |
| Pterygoid Plexus | Meninges | Middle Meningeal |
Back, Ribs, Neck, and Head
Choose from the articles below to learn about various back, rib, neck, or head injuries and disorders.
Featured Articles
- Ankylosing Spondylitis, Neurologic Perspective
- Ankylosing Spondylitis, Ophthalmologic Perspective
- Ankylosing Spondylitis, Orthopedic Perspective
- Ankylosing Spondylitis, Rheumatologic Perspective
- Back Pain
- Costochondritis
- Scoliosis
- Slipped Disk
- Spinal Stenosis
- Tailbone (Coccyx) Injury
- Temporomandibular Joint (TMJ) Syndrome
- Torticollis
- Whiplash
Articles
- Broken Jaw
- Broken Nose
- Chronic Fatigue Syndrome
- Chronic Pain
- Concussion
- Epidural Steroid Injection
- Facial Fracture
- Hematoma
- Internal Bleeding
- Leg Pain
- Lumbar Laminectomy
- Muscle Strain
- Neck Strain
- Shoulder and Neck Pain
- Sprains and Strains
- Vertebral Compression Fracture













No comments:
Post a Comment