Ovarian disease
Ovarian diseases can be classified as endocrine disorders or as a disorders of the reproductive system.
If the egg fails to release from the follicle in the ovary an ovarian cyst may form. Small ovarian cysts are common in healthy women. Some women have more follicles than usual (polycystic ovary syndrome), which inhibits the follicles to grow normally and this will cause cycle irregularities.
Other conditions include:
Ovarian cancer
Most (>90%) ovarian cancers are classified as "epithelial" and were believed to arise from the surface (epithelium) of the ovary.[1][2] However, recent evidence suggests that the Fallopian tube could also be the source of some ovarian cancers.[3] Since the ovaries and tubes are closely related to each other, it is hypothesized that these cells can mimic ovarian cancer.[4] Other types arise from the egg cells (germ cell tumor) or supporting cells (sex cord/stromal).
In 2004, in the United States, 25,580 new cases were diagnosed and 16,090 women died of ovarian cancer. The risk increases with age and decreases with pregnancy. Lifetime risk is about 1.6%, but women with affected first-degree relatives have a 5% risk. Women with a mutated BRCA1 or BRCA2 gene carry a risk between 25% and 60% depending on the specific mutation.[5] Ovarian cancer is the fifth leading cause of death from cancer in women and the leading cause of death from gynecological cancer.[6]
In early stages ovarian cancer is associated with abdominal distension.[7]
10-year relative survival ranges from 84.1% in stage IA to 10.4% in stage IIIC.[8]
Ovarian cancer causes non-specific symptoms.[9] Early diagnosis would result in better survival, on the assumption that stage I and II cancers progress to stage III and IV cancers (but this has not been proven). Most women with ovarian cancer report one or more symptoms such asabdominal pain or discomfort, an abdominal mass, bloating, back pain, urinary urgency,constipation, tiredness and a range of other non-specific symptoms, as well as more specific symptoms such as pelvic pain, abnormal vaginal bleeding or involuntary weight loss.[10][11][12]There can be a build-up of fluid (ascites) in the abdominal cavity.
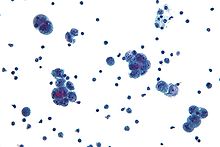
Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound. The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies (tissue samples for microscopic analysis) and look for cancer cells in the abdominal fluid. Treatment usually involves chemotherapy and surgery, and sometimes radiotherapy.[13]
In most cases, the cause of ovarian cancer remains unknown. Older women, and in those who have a first or second degree relative with the disease, have an increased risk. Hereditary forms of ovarian cancer can be caused by mutations in specific genes (most notably BRCA1 andBRCA2, but also in genes for hereditary nonpolyposis colorectal cancer). Infertile women and those with a condition called endometriosis, those who have never been pregnant and those who use postmenopausal estrogen replacement therapy are at increased risk. Use ofcombined oral contraceptive pills is a protective factor. The risk is also lower in women who have had their uterine tubes blocked surgically (tubal ligation).[14][15]
Contents[hide] |
[edit]Classification
Ovarian cancer is classified according to the histology of the tumor, obtained in a pathology report. Histology dictates many aspects of clinical treatment, management, and prognosis.
- Surface epithelial-stromal tumour, also known as ovarian epithelial carcinoma, is the most common type of ovarian cancer. It includes serous tumour, endometrioid tumor and mucinouscystadenocarcinoma.
- Sex cord-stromal tumor, including estrogen-producing granulosa cell tumor and virilizingSertoli-Leydig cell tumor or arrhenoblastoma, accounts for 8% of ovarian cancers.
- Germ cell tumor accounts for approximately 30% of ovarian tumors but only 5% of ovarian cancers, because most germ cell tumors are teratomas and most teratomas are benign (seeTeratoma). Germ cell tumor tends to occur in young women and girls. The prognosis depends on the specific histology of germ cell tumor, but overall is favorable.
- Mixed tumors, containing elements of more than one of the above classes of tumor histology.
| Percent of ovarian cancers in women age 20+ | Histology | 5 year RSR | |
|---|---|---|---|
| 89.7 | Surface epithelial-stromal tumor (Adenocarcinoma) | 54.4 | |
| 26.4 | Papillary serous cystadenocarcinoma | 21.0 | |
| 15.9 | "Borderline" adenocarcinoma (underestimated b/c short data collection interval) | 98.2 | |
| 12.6 | Adenocarcinoma, not otherwise specified | 18.3 | |
| 9.8 | Endometrioid tumor | 70.9 | |
| 5.8 | Serous cystadenocarcinoma | 44.2 | |
| 5.5 | Papillary | 21.0 | |
| 4.2 | Mucinous cystadenocarcinoma | 77.7 | |
| 4.0 | Clear-cell ovarian tumor | 61.5 | |
| 3.4 | Mucinous adenocarcinoma | 49.1 | |
| 1.3 | Cystadenocarcinoma | 50.7 | |
| 5.5 | Carcinoma | ||
| 4.1 | Carcinoma not otherwise specified | 26.8 | |
| 1.1 | Sex cord-stromal tumour | 87.8 | |
| 0.3 | Other carcinomas, specified | 37.3 | |
| 1.7 | Mullerian tumor | 29.8 | |
| 1.5 | Germ cell tumor | 91.0 | |
| 0.8 | Teratoma | 89.1 | |
| 0.5 | Dysgerminoma | 96.8 | |
| 0.3 | Other, specified | 85.1 | |
| 0.6 | Not otherwise specified | 23.0 | |
| 0.5 | Epidermoid (Squamous cell carcinoma) | 51.3 | |
| 0.2 | Brenner tumor | 67.9 | |
| 0.2 | Other, specified | 71.7 | |
Ovarian cancer can also be a secondary cancer, the result of metastasis from a primary cancer elsewhere in the body. 7% of ovarian cancers are due to metastases while the rest are primary cancers. Common primary cancers are breast cancer and gastrointestinal cancer(a common mistake is to name all peritoneal metastases from any gastrointestinal cancer as Krukenberg cancer [citation needed], but this is only the case if it originates from primary gastric cancer). Surface epithelial-stromal tumor can originate in the peritoneum (the lining of the abdominal cavity), in which case the ovarian cancer is secondary to primary peritoneal cancer, but treatment is basically the same as for primary surface epithelial-stromal tumor involving the peritoneum. [citation needed]
[edit]Staging
Ovarian cancer staging is by the FIGO staging system and uses information obtained after surgery, which can include a total abdominalhysterectomy, removal of (usually) both ovaries and fallopian tubes, (usually) the omentum, and pelvic (peritoneal) washings for cytopathology. The AJCC stage is the same as the FIGO stage.
- Stage I - limited to one or both ovaries
- IA - involves one ovary; capsule intact; no tumor on ovarian surface; no malignant cells in ascites or peritoneal washings
- IB - involves both ovaries; capsule intact; no tumor on ovarian surface; negative washings
- IC - tumor limited to ovaries with any of the following: capsule ruptured, tumor on ovarian surface, positive washings
- Stage II - pelvic extension or implants
- IIA - extension or implants onto uterus or fallopian tube; negative washings
- IIB - extension or implants onto other pelvic structures; negative washings
- IIC - pelvic extension or implants with positive peritoneal washings
- Stage III - microscopic peritoneal implants outside of the pelvis; or limited to the pelvis with extension to the small bowel or omentum
- IIIA - microscopic peritoneal metastases beyond pelvis
- IIIB - macroscopic peritoneal metastases beyond pelvis less than 2 cm in size
- IIIC - peritoneal metastases beyond pelvis > 2 cm or lymph node metastases
- Stage IV - distant metastases to the liver or outside the peritoneal cavity
Para-aortic lymph node metastases are considered regional lymph nodes (Stage IIIC).
[edit]Symptoms
[edit]Accuracy of symptoms
Two case-control studies, both subject to results being inflated by spectrum bias, have been reported. The first found that women with ovarian cancer had symptoms of increased abdominal size, bloating, urge to pass urine and pelvic pain.[12] The smaller, second study found that women with ovarian cancer had pelvic/abdominal pain, increased abdominal size/bloating, and difficulty eating/feeling full.[16] The latter study created a symptom index that was considered positive if any of the six (6) symptoms "occurred >12 times per month but were present for <1 year". For early-stage disease, they reported a 57% sensitivity and 87% to 90% specificity.
[edit]Consensus statement
In 2007, the Gynecologic Cancer Foundation, Society of Gynecologic Oncologists and American Cancer Society originated the following consensus statement regarding the symptoms of ovarian cancer.[17]
Ovarian cancer is called a “silent killer” because symptoms were not thought to develop until the disease had advanced and the chance of cure or remission poor. However, the following symptoms are much more likely to occur in women with ovarian cancer than women in the general population. These symptoms include:
- Bloating
- Pelvic or abdominal pain
- Pain in the back or legs
- Diarrhea, gas, nausea, constipation, indigestion
- Difficulty eating or feeling full quickly
- Urinary symptoms (urgency or frequency)
- Pain during sex
- Abnormal vaginal bleeding
- Trouble breathing
Women with ovarian cancer report that symptoms are persistent and represent a change from normal for their bodies. The frequency and/or number of such symptoms are key factors in the diagnosis of ovarian cancer. Several studies show that even early stage ovarian cancer can produce these symptoms. Women who have these symptoms almost daily for more than a few weeks should see their doctor, preferably a gynecologist. Prompt medical evaluation may lead to detection at the earliest possible stage of the disease. Early stage diagnosis is associated with an improved prognosis.
Several other symptoms have been commonly reported by women with ovarian cancer. These symptoms include fatigue, indigestion, back pain, pain with intercourse, constipation and menstrual irregularities. However, these other symptoms are not as useful in identifying ovarian cancer because they are also found in equal frequency in women in the general population who do not have ovarian cancer. [citation needed]
[edit]Cause
The exact cause is usually unknown. The risk of developing ovarian cancer appears to be affected by several factors. The more children a woman has, the lower her risk of ovarian cancer. Early age at first pregnancy, older age of final pregnancy and the use of low dose hormonal contraception have also been shown to have a protective effect. Ovarian cancer is reduced in women after tubal ligation. [citation needed]
[edit]Hormones
The relationship between use of oral contraceptives and ovarian cancer was shown in a summary of results of 45 case-control and prospective studies. Cumulatively these studies show a protective effect for ovarian cancers. Women who used oral contraceptives for 10 years had about a 60% reduction in risk of ovarian cancer. (risk ratio .42 with statistical significant confidence intervals given the large study size, not unexpected). This means that if 250 women took oral contraceptives for 10 years, 1 ovarian cancer would be prevented. This is by far the largest epidemiological study to date on this subject (45 studies, over 20,000 women with ovarian cancer and about 80,000 controls).[18]
The link to the use of fertility medication, such as Clomiphene citrate, has been controversial. An analysis in 1991 raised the possibility that use of drugs may increase the risk of ovarian cancer. Several cohort studies and case-control studies have been conducted since then without demonstrating conclusive evidence for such a link.[19] It will remain a complex topic to study as the infertile population differs in parityfrom the "normal" population.
[edit]Genetics
There is good evidence that in some women genetic factors are important. Carriers of certain mutations of the BRCA1 or the BRCA2 gene are notably at risk. The BRCA1 and BRCA2 genes account for 5%-13% of ovarian cancers[20] and certain populations (e.g. Ashkenazi Jewishwomen) are at a higher risk of both breast cancer and ovarian cancer, often at an earlier age than the general population. [citation needed]Patients with a personal history of breast cancer or a family history of breast and/or ovarian cancer, especially if diagnosed at a young age, may have an elevated risk.
A strong family history of uterine cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known ashereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch II syndrome), which confers a higher risk for developing ovarian cancer. Patients with strong genetic risk for ovarian cancer may consider the use of prophylactic, i.e. preventative, oophorectomy after completion of childbearing. [citation needed]Australia being member of International Cancer Genome Consortium is leading efforts to map ovarian cancer's complete genome.
[edit]Alcohol
A pooled analysis of ten (10) prospective cohort studies conducted in a number of countries and including 529,638 women found that neither total alcohol consumption nor alcohol from drinking beer, wine or spirits was associated with ovarian cancer risk."[21] The results of a case-control study in the region of Milan, Italy, "suggests that relatively elevated alcohol intake (of the order of 40 g per day or more) may cause a modest increase of epithelial ovarian cancer risk"[22]. "Associations were also found between alcohol consumption and cancers of the ovary and prostate, but only for 50 g and 100 g a day."[23] "Statistically significant increases in risk also existed for cancers of the stomach, colon, rectum, liver, female breast, and ovaries."[24]
[edit]Other
A Swedish study, which followed more than 61,000 women for 13 years, has found a significant link between milk consumption and ovarian cancer. According to the BBC, "[Researchers] found that milk had the strongest link with ovarian cancer—those women who drank two or more glasses a day were at double the risk of those who did not consume it at all, or only in small amounts." [25] Recent studies have shown that women in sunnier countries have a lower rate of ovarian cancer, which may have some kind of connection with exposure to Vitamin D.[26]
Other factors that have been investigated, such as talc use,[27] asbestos exposure, high dietary fat content, and childhood mumps infection, are controversial[citation needed] and have not been definitively proven; moreover, such risk factors may in some cases be more likely to be correlated with cancer in individuals with specific genetic makeups.[28]
[edit]Diagnosis
Ovarian cancer at its early stages(I/II) is difficult to diagnose until it spreads and advances to later stages (III/IV). This is because most symptoms are non-specific and thus of little use in diagnosis.[29]
When an ovarian malignancy is included in the list of diagnostic possibilities, a limited number of laboratory tests are indicated. A complete blood count (CBC) and serum electrolyte test should be obtained in all patients.
The serum BHCG level should be measured in any female in whom pregnancy is a possibility. In addition, serum alpha-fetoprotein (AFP) and lactate dehydrogenase (LDH) should be measured in young girls and adolescents with suspected ovarian tumors because the younger the patient, the greater the likelihood of a malignant germ cell tumor.
A blood test called CA-125 is useful in differential diagnosis and in follow up of the disease, but it by itself has not been shown to be an effective method to screen for early-stage ovarian cancer due to its unacceptable low sensitivity and specificity. However, this is the only widely-used marker currently available.
Current research is looking at ways to combine tumor markers proteomics along with other indicators of disease (i.e. radiology and/or symptoms) to improve accuracy. The challenge in such an approach is that the very low population prevalence of ovarian cancer means that even testing with very high sensitivity and specificity will still lead to a number of false positive results (i.e. performing surgical procedures in which cancer is not found intra-operatively). However, the contributions of proteomics are still in the early stages and require further refining. Current studies on proteomics mark the beginning of a paradigm shift towards individually tailored therapy.[citation needed]
A pelvic examination and imaging including CT scan[citation needed] and trans-vaginal ultrasound are essential. Physical examination may reveal increased abdominal girth and/or ascites (fluid within the abdominal cavity). Pelvic examination may reveal an ovarian or abdominal mass. The pelvic examination can include a rectovaginal component for better palpation of the ovaries. For very young patients, magnetic resonance imaging may be preferred to rectal and vaginal examination.
To definitively diagnose ovarian cancer, a surgical procedure to take a look into the abdomen is required. This can be an open procedure (laparotomy, incision through the abdominal wall) or keyhole surgery (laparoscopy). During this procedure, suspicious areas will be removed and sent for microscopic analysis. Fluid from the abdominal cavity can also be analysed for cancerous cells. If there is cancer, this procedure can also determine its spread (which is a form of tumor staging).
[edit]Prevention
There are a number of ways to reduce or eliminate the risk of ovarian cancer. Pregnancy before the age of 25 as well as breastfeeding provides some reduction in risk. Tubal ligation and hysterectomy reduce the risk and removal of both tubes and ovaries (bilateral salpingo-oophorectomy) dramatically reduces the risk of not only ovarian cancer but breast cancer also[30]. The use of oral contraceptives (birth control pills) for five years or more decreases the risk of ovarian cancer in later life by 50%.[31]
[edit]Screening
Routine screening of the general population is not recommended by any professional society. This includes the U.S. Preventive Services Task Force, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the National Comprehensive Cancer Network.[32]
No trial has shown improved survival for women undergoing screening.[32]
Screening tests include the CA-125 marker, transvaginal ultrasound, and combinations of markers such as OvaSure (LabCorp). A definitive diagnosis requires surgical excision of the ovaries and fallopian tubes, so a positive screening test must be followed up by surgery.[32]
The purpose of screening is to discover ovarian cancer in early stages, when it is more curable, on the hypothesis that early-stage cancer develops into later-stage cancer. However, it is not known whether early stage ovarian cancer evolves to later stage cancer, or whether stage III (peritoneal cavity involvement) arises as a diffuse process.[32]
The goal of ovarian cancer screening is to detect ovarian cancer at stage I.[33] Several large studies are ongoing, but none have recommended screening.[34] In 2009, however, Menon et al. reported from the UKCTOCS that utilizing mutimodal screening, in essence first performing annual CA-125 testing, followed by ultrasound imaging on the secondary level, the positive predictive value was 35.1% for primary invasive epithelial ovarian and tubal carcinoma, making such screening feasible.[35] However, it remains to be seen if such screening is effective to reduce mortality.
[edit]Management
| This article may require cleanup to meet Wikipedia's quality standards. Please improve this article if you can. (January 2008) |
Surgical treatment may be sufficient for malignant tumors that are well-differentiated and confined to the ovary. Addition of chemotherapy may be required for more aggressive tumors that are confined to the ovary. For patients with advanced disease a combination of surgical reduction with a combination chemotherapy regimen is standard. Borderline tumors, even following spread outside of the ovary, are managed well with surgery, and chemotherapy is not seen as useful.
Surgery is the preferred treatment and is frequently necessary to obtain a tissue specimen for differential diagnosis via its histology. Surgery performed by a specialist in gynecologic oncology usually results in an improved result[36]. Improved survival is attributed to more accurate staging of the disease and a higher rate of aggressive surgical excision of tumor in the abdomen by gynecologic oncologists as opposed to general gynecologists and general surgeons.
The type of surgery depends upon how widespread the cancer is when diagnosed (the cancer stage), as well as the presumed type and grade of cancer. The surgeon may remove one (unilateral oophorectomy) or both ovaries (bilateral oophorectomy), the fallopian tubes (salpingectomy), and the uterus (hysterectomy). For some very early tumors (stage 1, low grade or low-risk disease), only the involved ovary and fallopian tube will be removed (called a "unilateral salpingo-oophorectomy," USO), especially in young females who wish to preserve their fertility.
In advanced malignancy, where complete resection is not feasible, as much tumor as possible is removed (debulking surgery). In cases where this type of surgery is successful (i.e. < 1 cm in diameter of tumor is left behind ["optimal debulking"]), the prognosis is improved compared to patients where large tumor masses (> 1 cm in diameter) are left behind. Minimally invasive surgical techniques may facilitate the safe removal of very large (greater than 10 cm) tumors with fewer complications of surgery.[37]
Chemotherapy has been a general standard of care for ovarian cancer for decades, although with highly variable protocols.[38] Chemotherapy is used after surgery to treat any residual disease, if appropriate. This depends on the histology of the tumor; some kinds of tumor (particularly teratoma) are not sensitive to chemotherapy. In some cases, there may be reason to perform chemotherapy first, followed by surgery.
For patients with stage IIIC epithelial ovarian adenocarcinomas who have undergone successful optimal debulking, a recent clinical trial demonstrated that median survival time is significantly longer for patient receiving intraperitoneal (IP) chemotherapy.[39] Patients in this clinical trial reported less compliance with IP chemotherapy and fewer than half of the patients received all six cycles of IP chemotherapy. Despite this high "drop-out" rate, the group as a whole (including the patients that didn't complete IP chemotherapy treatment) survived longer on average than patients who received intravenous chemotherapy alone.
Some specialists believe the toxicities and other complications of IP chemotherapy will be unnecessary with improved IV chemotherapy drugs currently being developed.
Although IP chemotherapy has been recommended as a standard of care for the first-line treatment of ovarian cancer, the basis for this recommendation has been challenged.[40]
Radiation therapy is not effective for advanced stages because when vital organs are in the radiation field, a high dose cannot be safely delivered.
[edit]Prognosis
Ovarian cancer usually has a poor prognosis. It is disproportionately deadly because it lacks any clear early detection or screening test, meaning that most cases are not diagnosed until they have reached advanced stages. More than 60% of patients presenting with this cancer already have stage III or stage IV cancer, when it has already spread beyond the ovaries. Ovarian cancers shed cells into the naturally occurring fluid within the abdominal cavity. These cells can then implant on other abdominal (peritoneal) structures, included the uterus,urinary bladder, bowel and the lining of the bowel wall (omentum [disambiguation needed]) forming new tumor growths before cancer is even suspected.
The five-year survival rate for all stages of ovarian cancer is 45.5%. For cases where a diagnosis is made early in the disease, when the cancer is still confined to the primary site, the five-year survival rate is 92.7%.[41]
Germ cell tumors of the ovary have a much better prognosis than other ovarian cancers, in part because they tend to grow rapidly to a very large size, hence they are detected sooner.[citation needed]
[edit]Complications
- Spread of the cancer to other organs
- Progressive function loss of various organs
- Ascites (fluid in the abdomen)
- Intestinal obstructions
These cells can implant on other abdominal (peritoneal) structures, including the uterus, urinary bladder, bowel, lining of the bowel wall (omentum) and, less frequently, to the lungs.
[edit]Epidemiology
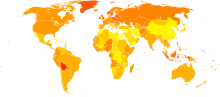
The exact cause is usually unknown. The disease is more common in industrialized nations, with the exception of Japan. In the United States, females have a 1.4% to 2.5% (1 out of 40-60 women) lifetime chance of developing ovarian cancer. Older women are at highest risk. [citation needed] More than half of the deaths from ovarian cancer occur in women between 55 and 74 years of age and approximately one quarter of ovarian cancer deaths occur in women between 35 and 54 years of age.
[edit]In other animals
Ovarian tumors have been reported in mares. Reported tumor types include teratoma,[43][44]cystadenocarcinoma,[45] and particularly granulosa cell tumor.[46][47][48][49][50]
[edit]See also
Luteoma
Luteoma is a rare tumor of the ovaries.
It can be associated with female pseudohermaphroditism
Presentation
This type of ovarian tumor produces progesterone. The excess of this hormone produces the symptoms that accompany this disease.
Progesterone determines the modifications in the endometrium that block menstruation. The symptoms of this tumor simulate pregnancy.
[edit]Causes
This type of tumor derives from a previous folliculoma or thecoma that luteinization has endured, acquiring the ability to produce and to accumulate the hormone.
Hypogonadism
Hypogonadism is a medical term for decreased functional activity of the gonads.[1] The gonads (ovaries or testes) produce hormones (testosterone, estradiol, antimullerian hormone,progesterone, inhibin B, activin) and gametes (eggs or sperm).
Late-onset hypogonadism (LOH), Andropause or Androgen Decline in the Aging Male (ADAM), is a syndrome caused by a decline in gonadal production of testosterone in males that occurs with aging. This "male menopause" (also known by the coinage "manopause") can also cause hypogonadism. However, it occurs for certain men and not for the others
Symptoms
In men
- Effects of low testosterone in men may include: (not all are present in any single individual)[3] and[4]
- Poor libido (Low sexual desire)
- Fatigue (medical) always tired
- Muscle loss/atrophy
- Erectile Dysfunction
- Increasing abdominal fat
- Glucose intolerance (early diabetes)
- High Cholesterol/Lipid
- Poor sleep
- Difficulty concentrating
- Memory Loss-difficulty in choosing words in language
- Depression
- Anxiety
- Psychological and relationship problems
- Gynecomastia
- Hot flashes
- Decrease in growth of, or loss of, beard and body hair
- Loss of bone mass (osteoporosis)
- Irritability
- Infertility
- Shrinking of the testicles
- Decrease in firmness of testicles
- Frequent urination (polyuria) without infection/waking at night to urinate
- Achy muscles
- Night sweats
- Dry skin and/or cracking nails
[edit]In women
- Effects of low estrogen levels in women may include: (not all are present in any individual)[3] and[4]
- Hot flashes
- Irritability
- Poor libido
- Infertility
- Loss of, or failure to develop, Menstruation
- Loss of body hair
- Loss of bone mass (osteoporosis)
- Heart disease
- Sleep disturbances
- Symptoms of urinary bladder discomfort like frequency, urgency, frequent infections, lack of lubrication, discharge
- Shrinking of breasts
- loss of or nonexistent sense of smell
[edit]Diagnosis
[edit]In men
Low Testosterone can be identified through a simple blood test performed by a laboratory, ordered by a physician. This test is typically ordered in the morning hours, when levels are highest, but even in men over 60 levels can drop by as much as 13% during the day.[5]
Normal total testosterone levels range from 300 - 1000ng/dl[6]
Treatment is often prescribed for total testosterone levels below 350 ng/dl[7] If the serum total testosterone level is between 230 and 350 ng/dl, repeating the measurement of total testosterone with sex hormone-binding globulin (SHBG) to calculate free testosterone or free testosterone by equilibrium dialysis may be helpful. However, there are no widely accepted diagnoses or reference ranges for Free Testosterone or Bioavailable Testosterone due to large discrepancies in the reference ranges for these tests between different testing labs.
Blood testing
A position statement by The Endocrine Society has expressed dissatisfaction with the manner in which most assays for TT (Total Testosterone) and FT (Free Testosterone) are currently performed.[8][9] In particular, research has questioned the validity of commonly administered assays of FT by RIA.[10] The FAI (Free Androgen Index) has been found to be the worst predictor of Free Testosterone.[11]
[edit]In women
Similar to men, the LH and FSH will be used, particularly in women who believe they are in menopause. These levels change during a woman's normal menstrual cycle, so the history of having ceased menstruation coupled with high levels aids the diagnosis of being menopausal. Commonly, the post-menopausal woman is not called hypogonadal if she is of typical menopausal age. Contrast with a young woman or teen, who would have hypogonadism rather than menopause. This is because hypogonadism is an abnormality, whereas menopause is a normal change in hormone levels.
Hypogonadism is often discovered during evaluation of delayed puberty, but ordinary delay, which eventually results in normal pubertaldevelopment, wherein reproductive function is termed constitutional delay. It may be discovered during an infertility evaluation in either men or women.
[edit]Treatment
Male hypogonadism is most often treated with testosterone replacement therapy (TRT). Commonly-used testosterone replacement therapies include transdermal (through the skin) using a patch or gel, injections, or pellets. Oral testosterone is no longer used in the U.S. because it is broken down in the liver and rendered inactive. Like many hormonal therapies, changes take place over time. It may take as long as 2-3 months at optimum level to reduce the symptoms, particularly the wordfinding and cognitive dysfunction. Testosterone levels in the blood should be evaluated to ensure the increase is adequate. Levels between 500-700 ng/l are considered adequate for young, healthy men from 20 to 40 years of age, but the lower edge of the normal range is poorly defined and single testosterone levels alone cannot be used to make the diagnosis. Modern treatment may start with 200mg intramuscular testosterone, repeated every 10-14 days. Getting a blood level of testosterone on the 13th day will give a "trough" level, assisting the physician in deciding whether the correct dose is being given.
Recently some have reported using Arimidex, an aromatase inhibitor used in women for breast cancer, to decrease conversion of testosterone to estrogen in men, and increase serum testosterone levels.
While historically men with prostate cancer risk were warned against testosterone therapy, that has shown to be a myth.[12]
Other side effects can include an elevation of the hematocrit to levels that require blood to be withdrawn (phlebotomy) to prevent complications from it being "too thick". Another is that a man may have some growth in the size of the breasts (gynecomastia), though this is relatively rare. Finally, some physicians worry that Obstructive Sleep Apnea may worsen with testosterone therapy, and should be monitored.
For both men and women, an alternative to testosterone replacement is Clomifene treatment which can stimulate the body to naturally increase hormone levels while avoiding infertility and other side effects as a consequence of direct hormone replacement therapy.[14]
For women, estradiol and progesterone are replaced. Some types of fertility defects can be treated, others cannot. Some physicians will also give testosterone to women, mainly to increase libido.
[edit]Classification
Deficiency of sex hormones can result in defective primary or secondary sexual development, or withdrawal effects (e.g., prematuremenopause) in adults. Defective egg or sperm development results in infertility. The term hypogonadism is usually applied to permanent rather than transient or reversible defects, and usually implies deficiency of reproductive hormones, with or without fertility defects. The term is less commonly used for infertility without hormone deficiency. There are many possible types of hypogonadism and several ways to categorize them. Hypogonadism is also categorized by endocrinologists by the level of the reproductive system that is defective.Physicians measure gonadotropins (LH and FSH) to distinguish primary from secondary hypogonadism. In primary hypogonadism the LH and/or FSH are usually elevated, meaning the problem is in the testicles, whereas in secondary hypogonadism, both are normal or low, suggesting the problem is in the brain.
[edit]Affected system
- Hypogonadism resulting from defects of the gonads is traditionally referred to as primary hypogonadism. Examples include Klinefelter syndrome and Turner syndrome. Mumps is known to cause testicular failure, and in recent years has been immunized against in the US. A varicocele can reduce hormonal production as well.
- Hypogonadism resulting from hypothalamic or pituitary defects are termed secondary hypogonadism or central hypogonadism(referring to the central nervous system).
- Examples of Hypothalamic defects include Kallmann syndrome.
- Examples of Pituitary defects include hypopituitarism.
- An example of a hypogonadism resulting from the lack of hormone response is androgen insensitivity syndrome, where there are inadequate receptors to bind the testosterone, resulting in a female appearance despite XY chromosomes.
[edit]Primary or secondary
- Primary - defect is inherent within the gonad: eg. Noonan syndrome, Turner syndrome (45X,0), Klinefelter syndrome (47XXY), XX males with SRY gene
- Secondary - defect lies outside of the gonad: eg. Kallmann syndrome and Polycystic ovary syndrome, also called hypogonadotropic hypogonadism.[4]. Hemochromatosis and diabetes mellitus can be causes of this as well.
[edit]Congenital vs. acquired
- An example of congenital hypogonadism (present at birth) in females is Turner syndrome, and in males is Klinefelter syndrome. It is also one of the signs of CHARGE syndrome.
- An example of acquired hypogonadism is the Anabolic Steroids Induced Hypogonadism (ASIH), and childhood mumps. Additionally, there is some evidence men whose mothers ingested the endocrine disruptor diethylstilbestrol for potential miscarriage may have hypogonadism.
[edit]Hormones vs. fertility
Hypogonadism can involve just hormone production or just fertility, but most commonly involves both.
- Examples of hypogonadism that affect hormone production more than fertility are hypopituitarism and Kallmann syndrome; in both cases, fertility is reduced until hormones are replaced but can be achieved solely with hormone replacement.
- Examples of hypogonadism that affect fertility more than hormone production are Klinefelter syndrome and Kartagener syndrome.
[edit]Coping
Hypogonadism can have many psychological effects, especially in younger patients due to infertility and appearance. A supportive family that understands the condition is paramount, as well as psychological treatment. Possible treatments include the use of regular injections or the application of gels or ointments.
[edit]Testosterone and longevity
A longitudinal (18 year) study published by The Endocrine Society and funded by the National Institute on Aging and the American Heart Association stated: Men over 50 may not live as long if they have low testosterone. The study looked at death from any cause in nearly 800 men ages 50 to 91 years who were living in a southern California community and who participated in the Rancho Bernardo Study in the 1980s. At the beginning of the study, almost one-third of these men had suboptimal blood testosterone levels for men their age. The men with low testosterone levels had a 33 percent greater risk of death during the next 18 years than the men with higher testosterone. This difference was not explained by smoking, alcohol intake and level of physical activity or by pre-existing diseases such as diabetes or heart disease.[15]
The new study is the second report linking the deficiency of this sex hormone with increased death from all causes over time, said study author Gail Laughlin, PhD.
Hyperthecosis
Hyperthecosis is hyperplasia of the theca interna of the ovary.[1] It is when an area of luteinization occurs along with stromal hyperplasia. The luteinized cells produce androgens, which may lead to hirsutism and virilization (or masculinization).
Hematocolpos
Hematocolpos is a medical condition in which the vagina fills with menstrual blood. It is often caused by the combination of menstruation with an imperforate hymen. A related disorder is Hematometria, where the uterus fills with (menstrual) blood. This can be caused by a congenital stenosis of the cervix, or by a complication of a surgical treatment, with stenosis of the cervix.
Leukorrhea
Leukorrhea (US) or leucorrhoea (Commonwealth) is a medical term that denotes a thick, whitish or yellowish vaginal discharge.[1]
There are many causes of leukorrhea, the usual one being estrogen imbalance. The amount of discharge may increase due to vaginal infection or STDs, in which case it becomes more yellow and foul-smelling; it is usually a non-pathological symptom secondary to inflammatoryconditions of vagina or cervix.
Oophoritis
From Wikipedia, the free encyclopedia
| Oophoritis | |
|---|---|
| Classification and external resources | |
| ICD-10 | N70. |
| ICD-9 | 614.0-614.2 |
| DiseasesDB | 9748 |
| eMedicine | med/1672 |
| MeSH | D009869 |
Oophoritis is an inflammation of the ovaries.
It is often seen in combination with salpingitis (inflammation of the fallopian tubes).
Ovarian cyst
From Wikipedia, the free encyclopedia
| Ovarian cyst | |
|---|---|
| Classification and external resources | |
 Ovarian cyst | |
| ICD-10 | N83.0-N83.2 |
| ICD-9 | 620.0-620.2 |
| DiseasesDB | 9433 |
| eMedicine | med/1699 emerg/352 |
| MeSH | D010048 |
An ovarian cyst is any collection of fluid, surrounded by a very thin wall, within an ovary. Anyovarian follicle that is larger than about two centimeters is termed an ovarian cyst. An ovarian cyst can be as small as a pea, or larger than an orange.
Most ovarian cysts are functional in nature, and harmless (benign).[1] In the US, ovarian cysts are found in nearly all premenopausal women, and in up to 14.8% of postmenopausal women.[citation needed]
Ovarian cysts affect women of all ages. They occur most often, however, during a woman's childbearing years.
Some ovarian cysts cause problems, such as bleeding and pain. Surgery may be required to remove cysts larger than 5 centimeters in diameter.
Contents[hide] |
[edit]Classification
[edit]Functional cysts
Some, called functional cysts, or simple cysts, are part of the normal process of menstruation. They have nothing to do with disease, and can be treated. These types of cysts occur during ovulation. If the egg is not released, the ovary can fill up with fluid. Usually these types of cysts will go away after a few period cycles.
- Follicular cyst of ovary: One type of simple cyst, which is the most common type of ovarian cyst, is the graafian follicle cyst, or follicularcyst.
- Lutein cysts:
- Corpus luteum cyst: Another is a corpus luteum cyst (which may rupture about the time of menstruation, and take up to three months to disappear entirely).
- Theca lutein cyst
The term "hemorrhagic cyst" is used to describe cysts where significant quantities of blood have entered. "hemorrhagic follicular cyst" is classified under N83.0 in ICD-10, and "hemorrhagic corpus luteum cyst" is classified under N83.1.
[edit]Non-functional cysts
There are several other conditions affecting the ovary that are described as types of cysts, but are not usually grouped with the functional cysts. (Some of these are more commonly or more properly known by other names.) These include:
- Chocolate cyst of ovary: An endometrioma, endometrioid cyst, endometrial cyst, or chocolate cyst is caused by endometriosis, and formed when a tiny patch of endometrial tissue (the mucous membrane that makes up the inner layer of the uterine wall) bleeds, sloughs off, becomes transplanted, and grows and enlarges inside the ovaries.
- A polycystic-appearing ovary is diagnosed based on its enlarged size — usually twice normal —with small cysts present around the outside of the ovary. It can be found in "normal" women, and in women with endocrine disorders. An ultrasound is used to view the ovary in diagnosing the condition. Polycystic-appearing ovary is different from the polycystic ovarian syndrome, which includes other symptoms in addition to the presence of ovarian cysts.
[edit]Signs and symptoms
Some or all of the following symptoms[2] [3] [4] [5] [6] may be present, though it is possible not to experience any symptoms:
- Dull aching, or severe, sudden, and sharp pain or discomfort in the lower abdomen (one or both sides), pelvis, vagina, lower back, or thighs; pain may be constant or intermittent—this is the most common symptom
- Fullness, heaviness, pressure, swelling, or bloating in the abdomen
- Breast tenderness
- Pain during or shortly after beginning or end of menstrual period.
- Irregular periods, or abnormal uterine bleeding or spotting
- Change in frequency or ease of urination (such as inability to fully empty the bladder), or difficulty with bowel movements due to pressure on adjacent pelvic anatomy
- Weight gain
- Nausea or vomiting
- Fatigue
- Infertility
- Increased level of hair growth
- Increased facial hair or body hair
- Headaches
- Strange pains in ribs, which feel muscular
- Bloating
- Strange nodules that feel like bruises under the layer of skin
[edit]Diagnosis
Ovarian cysts are usually diagnosed by either ultrasound or CT scan.
[edit]Treatment
Treatment for cysts depends on the size of the cyst and symptoms. For small, asymptomatic cysts, the wait and see approach with regular check-ups will most likely be recommended.
Pain caused by ovarian cysts may be treated with:
- pain relievers, including acetaminophen (Tylenol), nonsteroidal anti-inflammatory drugs such asibuprofen (Motrin, Advil), or narcotic pain medicine (by prescription) may help reduce pelvic pain.[8] NSAIDs usually work best when taken at the first signs of the pain.
- a warm bath, or heating pad, or hot water bottle applied to the lower abdomen near the ovaries can relax tense muscles and relieve cramping, lessen discomfort, and stimulate circulation and healing in the ovaries.[9] Bags of ice covered with towels can be used alternately as cold treatments to increase local circulation.[10]
- combined methods of hormonal contraception such as the combined oral contraceptive pill – the hormones in the pills may regulate the menstrual cycle, prevent the formation of follicles that can turn into cysts, and possibly shrink an existing cyst. (American College of Obstetricians and Gynecologists, 1999c; Mayo Clinic, 2002e)[8]
Also, limiting strenuous activity may reduce the risk of cyst rupture or torsion.
Cysts that persist beyond two or three menstrual cycles, or occur in post-menopausal women, may indicate more serious disease and should be investigated through ultrasonography and laparoscopy, especially in cases where family members have had ovarian cancer. Such cysts may require surgical biopsy. Additionally, a blood test may be taken before surgery to check for elevated CA-125, a tumor marker, which is often found in increased levels in ovarian cancer, although it can also be elevated by other conditions resulting in a large number of false positives.[11]
For more serious cases where cysts are large and persisting, doctors may suggest surgery. Some surgeries can be performed to successfully remove the cyst(s) without hurting the ovaries, while others may require removal of one or both ovaries.[12][13]
Poor ovarian reserve
From Wikipedia, the free encyclopedia
Poor ovarian reserve (also known as impaired ovarian reserve, premature ovarian aging or declining ovarian reserve) is a condition of low fertility characterized by 1): low numbers of remaining oocytes in the ovaries or 2) possibly impaired preantral oocyte development or recruitment. Recent research suggests that premature ovarian aging and premature ovarian failure (aka primary ovarian insufficiency) may represent a continuum of premature ovarian senescence.[1] It is usually accompanied by high FSH (follicle stimulating hormone) levels.
Quality of the eggs (oocytes) may also be impaired as a 1989 study by Scott et al. of 758 IVF cycles showed a dramatic decline in implantation rates between high (> 25 mIU/mL) and low day three FSH (<15 mIU/mL) women even though the ages of the women were equivalent between the two groups (mean age 35 years).[2][3] However, other studies show no association with elevated FSH levels and genetic quality of embryos after adjusting for age. The decline in quality was age related, not FSH related as the younger women with high day three FSH levels had higher live birth rates than the older women with high FSH. There was no significant difference in genetic embryo quality between same aged women regardless of FSH levels.[4][5] A 2008 study concluded that diminished reserve did not affect the quality of oocytes and any reduction in quality in diminished reserve women was age related. [6] One expert concluded: in young women with poor reserve when eggs are obtained they have near normal rates of implantation and pregnancy rates, but they are at high risk for IVF cancellation; if eggs are obtained, pregnancy rates are typically better than in older woman with normal reserve. However, if the FSH level is extremely elevated these conclusions are likely not applicable. [7]
Contents[hide] |
[edit]Etiology
- Natural decline of ovarian reserve due to age[8].
- Idiopathic.
- Genetic factors, such as fragile x syndrome. Approximately 20-28% of women with an FMR1 premutation (55-200 CGG repeats) experience fragile x primary ovarian insufficiency (POI) and another 23% experience early menopause (i.e., menopause before the age of forty five).[9]
- Autoimmune disorders.
- Adrenal gland impairment.
- Iatrogenic, e.g., due to radiation, chemotherapy or surgery, such as laserization of the surface of the ovary to treat endometriosis. Excessive laparoscopic ovarian drilling has been reported to cause premature ovarian failure.[10] (The primordial follicles are located in the thin outer one-millimeter layer of the ovary.) [11]
[edit]Diagnosis
There is some controversy as the accuracy of the tests used to predict poor ovarian reserve. One systematic review concluded that the accuracy of predicting the occurrence of pregnancy is very limited. When a high threshold is used, to prevent couples from wrongly being refused IVF, only approximately 3% of IVF-indicated cases are identified as having unfavourable prospects in an IVF treatment cycle. Also, the review concluded the use of any ORT (Ovarian Reserve Testing) for outcome prediction cannot be supported. [12] Also Centers for Disease Control and Prevention statistics show that the success rates for IVF with diminished ovarian reserve vary widely between IVF centers.[13]
[edit]Follicle stimulating hormone (FSH)
Elevated serum follicle stimulating hormone (FSH) level measured on day three of the menstrual cycle. (First day of period flow is counted as day one. Spotting is not considered start of period.) If a lower value occurs from later testing, the highest value is considered the most predictive. FSH assays can differ somewhat so reference ranges as to what is normal, premenopausal or menopausal should be based on ranges provided by the laboratory doing the testing. Estradiol (E2) should also be measured as women who ovulate early may have elevated E2 levels above 80 pg/mL (due to early follicle recruitment, possibly due to a low serum inhibin B level) which will mask an elevated FSH level and give a false negative result.[14]
High FSH strongly predicts poor IVF response in older women, less so in younger women. One study showed an elevated basal day-three FSH is correlated with diminished ovarian reserve in women aged over 35 years and is associated with poor pregnancy rates after treatment of ovulation induction(6% versus 42%). [15]
The rates for spontaneous pregnancy in older women with elevated FSH levels have not been studied very well and the spontaneous pregnancy success rate, while low, may be underestimated due to non reporting bias, as most infertility clinics will not accept women over the age of forty with FSH levels in the premenopausal range or higher.[citation needed]
A woman can have a normal day-three FSH level yet still respond poorly to ovarian stimulation and hence can be considered to have poor reserve. Thus, another FSH-based test is often used to detect poor ovarian reserve: the clomid challenge test, also known as CCCT(clomiphene citrate challenge test).
[edit]Antral follicle count
Transvaginal ultrasonography can be used to determine antral follicle count (AFC). This is an easy-to-perform and noninvasive method (but there may be some discomfort). Several studies show this test to be more accurate than basal FSH testing for older women (< 44 years of age) in predicting IVF outcome.[16] This method of determining ovarian reserve is recommended by Dr. Sherman J. Silber, author and medical director of the Infertility Center of St. Louis.[17]
| Antral Follicle Count (Per Ovary [See comment below as these figures are under dispute.]) | Median Years to Last Child | Median Years to Menopause |
|---|---|---|
| 5 | __ | 7.3 |
| 10 | 4.2 | 12.9 |
| 15 | 9.3 | 18.4 |
| 20 | 14.8 | 24.0 |
Note, the above table from Silber's book may be in error as it has no basis in any scientific study, and contradicts data from Broekmans, et al. 2004 study. [20] The above table closely matches Broekmans' data only if interpreted as the total AFC of both ovaries. Only antral follicles that were 2-10 mm in size were counted in Broekmans' study.
Age and AFC and Age of Loss of Natural Fertility (See Broekmans, et al. [2004])
| Antral Follicle Count (Both Ovaries) | Age at Time of Count | Age of Loss of Natural Fertility |
|---|---|---|
| 6 | 30 | 29-33 |
| 6 | 35 | 33-38 |
| 6 | 40 | 38-41 |
| 10 | 30 | 33-38 |
| 10 | 35 | 38-41 |
| 15 | 30 | 38-41 (closer to 41) |
| Antral Follicle Count | Significance |
|---|---|
| < 4 | Poor reserve |
| 4-7 | Low count, high dosage of FSH required |
| 8-12 | Slightly reduced reserve |
| > 12 | Normal |
[edit]Other
- Declining serum levels of anti-müllerian hormone. Recent studies have validated the use of serum AMH levels as a marker for the quantitative aspect of ovarian reserve. Because of the lack of cycle variations in serum levels of AMH, this marker has been proposed to be used as part of the standard diagnostic procedures to assess ovarian dysfunctions, such as premature ovarian failure. One study has shown AMH to be a better marker than basal FSH for women with proven (prior) fertility in measuring age related decline in ovarian reserve.[22]
- Inhibin B blood level. Inhibin B levels tend to decline in advanced reproductive aged women due to both fewer follicles and decreased secretion by the granulosa cells. Inhibin B levels start to rise around day zero and low day three levels are associated with poor IVF outcome.[23][24]
- Ultrasound measurement of ovarian volume. Lass and Brinsden (1999) report that the correlation between ovarian volume and follicular density appears to only hold in women ≥ 35 years of age.[25]
- Dynamic Assessment Following GnRH-a Administration (GAST). This test measures the change in serum estradiol levels between cycle day two and three after administration of one mg of subcutaneous leuprolide acetate, a gonadatropin releasing hormone agonist. Patients with estradiol elevations by day two followed by a decline by day three had improved implantation and pregnancy rates than those patients with either no rise in estradiol or persistently elevated estradiol levels.[26]
- Home testing of FSH urine concentration to alert a woman to possible impaired ovarian reserve became possible in June 2007 with the introduction of Fertell in the United States and UK, which claims a 95% equivalence to standard serum marker results.[27]
[edit]Treatment
Variable success rate with treatment, very few controlled studies, mostly case reports. Treatment success strongly tends to diminish with age and degree of elevation of FSH.
- Donor oocyte. Oocyte donation is the most successful method for producing pregnancy in perimenopausal women. In the UK the use of donor oocytes after natural menopause is controversial.[28] A 1995 study reported that women age fifty or higher experience similar pregnancy rates after oocyte donation as younger women. They are at equal risk for multiple gestation as younger women. In addition, antenatal complications were experienced by the majority of patients, and that high risk obstetric surveillance and care is vital.[29]
- Natural or Mini-IVF, but without the use of hCG to induce ovulation, instead the GnRH agonist Synarel® (nafarelin acetate) in a diluted form is taken as a nasal spray to induce ovulation. Human chorionic gonadotropin (hCG) has a long half life and may stimulate (luteinize) small follicles prematurely and cause them to become cysts. Whereas nafarelin acetate in a nasal spray induces a short lived LH surge that is high enough to induce ovulation in large follicles, but too short lived to adversely affect small follicles. This increases the likelihood of the small follicles and oocytes therein developing normally for upcoming cycles and also allows the woman to cycle without taking a break and consequently increases the probability of conception in poor ovarian reserve women and advanced reproductive aged women.[30]
- Pretreatment with 50 mcg ethinyl estradiol three times a day for two weeks, followed by recombinant FSH 200 IU/day subcutaneously. Ethinyl estradiol treatment was maintained during FSH stimulation. When at least one follicle reached 18mm in diameter and serum estradiol was greater or equal to 150 pg/ML ovulation was induced with an intramuscular injection of 10,000 IU of hCG (human chorionic gonadotropin hormone). For luteal phase support 5,000 IU of hCG was administered every 72 hours. Out of 25 patients 8 ovulated and 4 became pregnant. In the control group there were no ovulations. The patients ranged in age between 24 and 39 years with an average age of 32.7. All women had amenorrhea for at least 6 months (average 16.75 months) and FSH levels greater or equal than 40 mIU/mL (average FSH 68 mIU/ML). The researchers believe this protocol would work for women in early post menopause as well.[31]
- Ethinyl estradiol or other synthetic estrogens along with luteal phase progesterone (twice daily 200 mg vaginal suppositories) and estradiol support. Ethinyl estradiol lowers high FSH levels which then, it is theorized, up regulates FSH receptor sites and restores sensitivity to FSH. Ethinyl estradiol also has the advantage that it does not interfere with the measurement of serum levels of endogenous estradiol. During the luteal phase the FSH levels should be kept low for subsequent cycles, thus the phase is supplemented with 4 mg[32] oral estradiol. Since conception may have occurred estradiol is used instead of the synthetic ethinyl estradiol. [33][34][35][36][37]
- Cyclical hormone replacement therapy.[38]
- The following protocols have shown promise: high dose gonadoropins, flare up GnRH-a protocol (standard or microdose), stop protocols, short protocol, natural cycle or modified natural cycle and low dose hCG during the beginning of the stimulation protocol.[39]
- Gonadotropin-releasing hormone agonist/antagonist conversion with estrogen priming (AACEP) protocol. Fisch, Keskintepe and Sher report 35% (14 out of 40) ongoing gestation in women with elevated FSH levels (all women had prior IVF and poor quality embryos); among women aged 41-42 the ongoing gestation rate was 19% (5 out of 26).[40]
- DHEA: Recent clinical trial by the Center for Human Reproduction in New York showed significant effectiveness.[41][42][43] Leonidas and Eudoxia Mamas report six cases of premature ovarian failure. After two to six months of treatment with DHEA (Two 25 mg capsules daily in five cases and three 25 mg capsules daily in one case.) all women conceived. One delivered via C-section, one aborted at 7 weeks and the remaining four were reported at 11 to 27 weeks gestation. Ages were from 37 to 40. FSH levels were from 30 to 112 mIU/mL. Ammenorhea ranged from 9 to 13 months.[44] In addition, there is strong evidence that continuous micronized DHEA 25 mg TID reduces miscarriage and aneuploidy rates, especially above age 35.[45]
- Glucocorticoid therapy. A recent (2007) randomized double blind study done in Egypt reported a statistically significant theurapeutic effect with dexamethasone pretreatment. Fifty-eight women with idiopathic premature ovarian failure and normal karyotype were divided into two groups of twenty-nine. The control group received placebo for twenty-eight days and then GnRH agonists plus gonadotropin therapy (hMG). The treatment group received dexamethasone for twenty-eight days (6 mg/ day) and then GnRH agonists plus gonadotropin therapy (hMG). (In both groups after the first twenty-eight days, and concurrent with the GnRH agonist treatment, the placebo or dexamethasone was gradually tapered off over ten days.) The treatment group had six ovulations and two pregnancies (p value of .02). The control group had three ovulations and no pregnancies.[46][47]
- A combined pentoxifylline-tocopherol treatment has been reported effective in improving uterine parameters in women with POF undergoing IVF with donor oocytes (IVF-OD). Three women with uterine hormonoresistance despite high estradiol (E2) plasma levels received treatment with 800 mg pentoxifylline and 1000 IU of vitamin E for at least nine months. Three frozen-thawed embryo transfers (ETs) resulted in two viable pregnancies. Mean endometrial thickness increased from 4.9 mm (with thin uterine crosses) to 7.4 mm with nice uterine crosses.[48][49] This treatment protocol has also reversed some cases of iatrogenic POF caused by full body radiation treatment.[50]
- TCM: There are reports in the medical literature of successful treatment with Traditional Chinese Medicine (TCM).[51] For example, a case history was published in 2003 by the Chang Gung Memorial Hospital in Taipei, Taiwan. Ovulation and pregnancy occurred after the administration of TCM medicine using concentrated extracts for a total of four nonconsecutive months in a 26 year old women with premature ovarian failure and secondary amenorrhea of eight years duration. Her FSH, LH and E2 levels were 80.4 mIU/mL, 19.6 mIU/mL and 25.8 pg/mL respectively. A modified version of zuoguiwan (左歸丸 restore the left pill) was prescribed for three months. After three months of treatment menstrual bleeding and a biphasic body temperature were noted. The patient then discontinued TCM therapy and at a new clinic commenced clomiphene citrate therapy. FSH and LH were still in the menopausal range (43 mIU/mL and 11 mIU/ml, respectively) after eights months of clomiphene citrate. Ovulation did not occur. She then returned to the first clinic and the same TCM treatment was resumed (one year after first commencing TCM treatment) and the patient conceived one month later and subsequently gave birth by Cesarean section to a healthy 3450 gram baby girl.[52]
[edit]Unproven treatments with possible merit
- Melatonin: One double blind study showed that extended treatment with melatonin lowered FSH levels (only in woman with low initial nocturnal melatonin levels) and in some cases restored normal menstruation in early menopausal women.[53] The authors state fertility was restored in the women with resumption of normal menstruation, however, no ultrasonography was done to verify follicular development and ovulation. One Japanese study (IVF-ET) showed improved fertilization rate (50.0% versus 22.8%, p < 0.01) and pregnancy rate (11/56 versus 6/59, result not statistically significant) in poor responders with treatment of 3 mg melatonin daily from 5th day of previous menstrual cycle.[54]
- Maca: One double blind, placebo-controlled study of eight menopausal women between the ages of 45 and 62 showed a statistically significant decline in serum FSH levels after eight months of treatment with oral administration of capsules containing 2000 mg pre-gelatinized dried and pulverized hypocotyls of Maca (Lepidium peruvianum Chacon). (See table below [55].) However, in perimenopausal women Maca elevated E2 and FSH.[56] Though such supplementation may have led to statistically significant changes in FSH, this may be less likely to have clinically meaningful impact. The reason is that many IVF studies show no live births with FSH > 17-20 and case reports of live births (i.e. not just pregnancy with a miscarriage) with an FSH >25 are exceptionally rare.
| Hormone | Start of Trial | After Placebo (1 month) | Maca (2 months) | Maca (8 months) |
|---|---|---|---|---|
| FSH mIU/mL ± SE | 54.3±1.22a | 59.7±1.35a | 47.3±0.93b | 39.3±0.90b |
| LH mIU/mL | 21.5±0.59a | 23.3±0.68a | 30.6±0.76b | 32.9±0.83b |
| PG (ng/mL) | 0.41±0.11a | 0.54±0.14a | 0.59±0.12a | 0.78±0.09b |
| E2 (pg/mL) | 32.9±3.72ab | 27.2±2.96a | 32.0±2.67ab | 35.7±2.09b |
Values in a row with unlike letters indicate significant difference at P<0.05.
SE = Standard Error of Mean
SE = Standard Error of Mean
- Homeopathy plus herbs, vitamins and lifestyle changes may possibly help. An article by Liz Lalor titled "Fertility Success using homeopathy" outlines a protocol that she states has been successful in forty out of fifty cases of infertility. Of note is that two of the ten that failed later conceived in one IVF cycle and she writes: "it was reported back to me that the doctors were very surprised at the quality and numbers of eggs as well as the health of the endometrium."[57]
[edit]Related animal research
- Recently, two publications have reported the renewal of ovarian follicles from germline stem cells[58][59]. Prior to these papers it was believed that the number of oocytes was fixed.
- While the primary cause of the end to menstrual cycles is the exhaustion of ovarian follicles, there is some evidence that a defect in thehypothalamus is critical in the transition from regular to irregular cycles. This is supported by at least one study in which transplantation of ovaries from old rats to young ovariectomized rats resulted in follicular development and ovulation. Also, electrical stimulation of the hypothalamus is capable of restoring reproductive function in aged animals. Due to the complex interrelationship among thehypothalamus, pituitary and ovaries (HPO axis) defects in the functioning of one level can cause defects on the other levels.[60]
[edit]Related conditions
- Premature ovarian failure: Defined as no menses for six months before the age of forty due to any cause. Often diagnosed by elevated gonadotropin (Follicle Stimulating Hormone and LH) levels. In some cases (more so in younger women) ovarian function and ovulation can spontaneously resume. With POF up to 50% of women may ovulate once in any given year and 5-10% may become pregnant. POF is often associated with autoimmune diseases.
- Premature menopause: A outdated synonym for premature ovarian failure. The term encompasses premature menopause due to any cause, including surgical removal of the ovaries for any reason. Early menopause and premature ovarian failure are no longer considered to be the same condition.
Ovarian torsion
From Wikipedia, the free encyclopedia
| Ovarian torsion | |
|---|---|
| Classification and external resources | |
 Arteries of the female reproductive tract: uterine artery, ovarian artery and vaginal arteries. (Ovary and ovarian artery visible in upper right.) | |
| ICD-10 | N83.5 |
| ICD-9 | 620.5 |
| DiseasesDB | 31120 |
| eMedicine | article/795994 |
Ovarian torsion (OT) refers to the rotation of the ovary to such a degree as to occlude theovarian artery and/or vein.
Contents[hide] |
[edit]Epidemiology
Accounts for about 3% of gynecologic emergencies. Is more common in younger females of reproductive years. Torsion occurs with slight predominance on the right.
[edit]Presentation
Patients with ovarian torsion often present with sudden onset of unilateral lower abdominal pain, often accompanied by nausea and vomiting. Exercise and sudden movement is often a precipitating event. Also, abnormalities in shape and size of the ovary may predispose to rotation. [1]
[edit]Pathophysiology
The development of an ovarian mass is related to the development of torsion. In the reproductive years, regular growth of large corpus luteal cysts are a risk factor for rotation. The mass effect of ovarian tumors is also a common cause of torsion. Torsion of the ovary actually occurs with torsion of the fallopian tube as well on their shared vascular pedicle.
[edit]Diagnosis
Ovarian torsion is difficult to diagnose accurately, and operation is often performed before certain diagnosis is made. A study at an Israelicobstetrics and gynaecology department found that preoperative diagnosis of ovarian torsion was confirmed in only 46% of patients.[4]
Lack of ovarian blood flow on Doppler sonography seems to be a good predictor of ovarian torsion. Women with pathologically low flow are more likely to have OT (77% vs. 29% in an Israelic study).[4] The sensitivity and specificity of abnormal ovarian flow for OT are 44% and 92%, respectively, with a positive and negative predictive value of 78% and 71%, respectively.[4]
[edit]Treatment
Conservative treatment of ovarian torsion includes laparoscopy to uncoil the torsed ovary and possibly oophoropexy to fixate the ovary which is likely to torse again. In severe cases, where blood flow is cut off to the ovary for an extended period of time, necrosis of the ovary can occur. In these cases the ovary must be surgically removed.
Follicle-stimulating hormone
Follicle-stimulating hormone (FSH) is a hormone found in humans and other animals. It is synthesized and secreted by gonadotrophs of the anterior pituitary gland. FSH regulates the development, growth, pubertal maturation, and reproductive processes of the body. FSH andLuteinizing hormone (LH) act synergistically in reproduction.
Contents[hide] |
[edit]Structure
FSH is a glycoprotein. Each monomeric unit is a protein molecule with a sugar attached to it; two of these make the full, functional protein. Its structure is similar to those of LH, TSH, andhCG. The protein dimer contains 2 polypeptide units, labeled alpha and beta subunits. Thealpha subunits of LH, FSH, TSH, and hCG are identical, and contain 92 amino acids. The beta subunits vary. FSH has a beta subunit of 118 amino acids (FSHB), which confers its specific biologic action and is responsible for interaction with the FSH-receptor. The sugar part of the hormone is composed of fucose, galactose, mannose, galactosamine, glucosamine, and sialic acid, the latter being critical for its biologic half-life. The half-life of FSH is 3-4 hours. Its molecular wt is 30000.
[edit]Genes
The gene for the alpha subunit is located on chromosome 6p21.1-23. It is expressed in different cell types. The gene for the FSH beta subunit is located on chromosome 11p13, and is expressed in gonadotropes of the pituitary cells, controlled by GnRH, inhibited by inhibin, and enhanced by activin.
[edit]Activity
FSH regulates the development, growth, pubertal maturation, and reproductive processes of the human body.
- In both males and females, FSH stimulates the maturation of germ cells.
- In males, FSH induces Sertoli cells to secrete inhibin and stimulates the formation of sertoli-sertoli tight junctions (zonula occludens).
- In females, FSH initiates follicular growth, specifically affecting granulosa cells. With the concomitant rise in inhibin B, FSH levels then decline in the late follicular phase. This seems to be critical in selecting only the most advanced follicle to proceed to ovulation. At the end of the luteal phase, there is a slight rise in FSH that seems to be of importance to start the next ovulatory cycle.
Like its partner LH, FSH release at the pituitary gland is controlled by pulses of gonadotropin-releasing hormone (GnRH). Those pulses, in turn, are subject to the oestrogen feed-back from the gonads.
[edit]Effects in females
FSH stimulates the growth and recruitment of immature Ovarian follicles in the ovary. In early (small) antral follicles, FSH is the major survival factor that rescues the follicles from apoptosis (programmed death of the somatic cells of the follicle and oocyte). In the luteal-follicle phase transition period the serum levels of progesterone and estrogen (primarily estradiol) decrease and no longer suppress the release of FSH, consequently FSH peaks at about day three (day one is the first day of menstrual flow). The cohort of small antral follicles is normally sufficiently in number to produce enough Inhibin B to lower FSH serum levels.
In addition, there is evidence that gonadotrophin surge-attenuating factor produced by small follicles during the first half of the follicle phase also exerts a negative feedback on pulsatile luteinizing hormone (LH) secretion amplitude, thus allowing a more favorable environment for follicle growth and preventing premature luteinization.[1]
(As a woman nears perimenopause the number of small antral follicles recruited in each cycle diminishes and consequently insufficient Inhibin B is produced to fully lower FSH and the serum level of FSH begins to rise.)
When the follicle matures and reaches 8-10 mm in diameter it starts to secrete significant amounts of estradiol. Normally in humans only one follicle becomes dominant and survives to grow to 18-30 mm in size and ovulate, the remaining follicles in the cohort undergo atresia. The sharp increase in estradiol production by the dominant follicle (possibly along with a decrease in gonadotrophin surge-attenuating factor) cause a positive effect on the hypothalamus and pituitary and rapid GnRH pulses occur and an LH surge results.
The increase in serum estradiol levels cause a decrease in FSH production by inhibiting GnRH production in the hypothalamus.[2] The decrease in serum FSH level causes the smaller follicles in the current cohort to undergo atresia as they lack sufficient sensitivity to FSH to survive. Occasionally two follicles reach the 10 mm stage at the same time by chance and as both are equally sensitive to FSH both survive and grow in the low FSH environment and thus two ovulations can occur in one cycle possibly leading to non identical (dizygotic) twins.
[edit]Effects in males
FSH stimulates maturation of seminiferous tubules and spermatogenesis.
FSH enhances the production of androgen-binding protein by the Sertoli cells of the testes by binding to FSH receptors on their basolateralmembranes,[3] and is critical for the initiation of spermatogenesis.
[edit]Measurement
Follicle stimulating hormone is typically measured on day three of a woman's cycle when the levels of estradiol (E2) and progesterone are at the lowest point of themenstrual cycle.
[edit]Disease states
[edit]High FSH levels
The most common reason for high serum FSH concentration is in a female who is undergoing or has recently undergone menopause. High levels of Follicle-Stimulating Hormone indicate that the normal restricting feedback from the gonad is absent, leading to an unrestricted pituitary FSH production.
If high FSH levels occur during the reproductive years, it is abnormal.
- Premature menopause also known as Premature Ovarian Failure
- Poor ovarian reserve also known as Premature Ovarian Aging
- Gonadal dysgenesis, Turner syndrome
- Castration
- Swyer syndrome
- Certain forms of CAH
- Testicular failure.
Most of these conditions are associated with subfertility and/or infertility. Therefore high FSH levels are an indication of subfertility and/or infertility.
[edit]Low FSH levels
Diminished secretion of FSH can result in failure of gonadal function (hypogonadism). This condition is typically manifested in males as failure in production of normal numbers of sperm. In females, cessation of reproductive cycles is commonly observed. Conditions with very low FSH secretions are:
- Polycystic Ovarian Syndrome
- Polycystic Ovarian Syndrome + Obesity + Hirsutism + Infertility
- Kallmann syndrome
- Hypothalamic suppression
- Hypopituitarism
- Hyperprolactinemia
- Gonadotropin deficiency
- Gonadal suppression therapy
[edit]Availability
FSH is available mixed with LH activity in various menotropins including more purified forms of urinary gonadotropins such as Menopur, as well as without LH activity as recombinant FSH (Gonal F, Follistim). It is used commonly in infertility therapy to stimulate follicular development, notably in IVF therapy, as well as with interuterine insemination (IUI). (See Gonadotropin Preparations.)




No comments:
Post a Comment