Vaginitis
From Wikipedia, the free encyclopedia
Not to be confused with Vaginismus.
| Vaginitis | |
|---|---|
| Classification and external resources | |
| ICD-10 | N76.0-N76.1 |
| ICD-9 | 616.1 |
| DiseasesDB | 14017 |
| eMedicine | med/3369 med/2358emerg/631 emerg/639 |
| MeSH | D014627 |
Vaginitis is an inflammation of the vagina.[1][2] It can result in discharge, itching and pain,[2] and is often associated with an irritation or infection of the vulva. It is usually due to infection.[1]
Contents[hide] |
[edit]Symptoms
A woman with this condition may have itching or burning and may notice a discharge.[3] In general, these are symptoms of vaginitis:
- irritation and/or itching of the genital area
- inflammation (irritation, redness, and swelling caused by the presence of extra immune cells) of the labia majora, labia minora, or perineal area
- vaginal discharge
- foul vaginal odor
- discomfort or burning when urinating
- pain/irritation with sexual intercourse
[edit]Causes
Vulvovaginitis can affect women of all ages and is very common. Specific forms of vaginitis are:
[edit]Infection
Infectious vaginitis accounts for 90% of all cases in reproductive age women and is represented by the triad:
- Candidiasis: vaginitis caused by Candida albicans (a yeast).
- Bacterial vaginosis: vaginitis caused by Gardnerella (a bacterium).
- Trichomoniasis: vaginitis caused by Trichomonas vaginalis (a parasitic protozoan).
Other less common infections are caused by gonorrhea, chlamydia, mycoplasma, herpes, campylobacter, improper hygiene, and someparasites.[4]
Vaginal infection are often (varies between countries between 20 to 40% of vaginal infections) a mix of various etiologies, which present challenging cases for treatment. Indeed, when only one cause is treated, the other pathogens can gain in resistance and induce relapses and recurrences. The key factor is therefore to get a precise diagnosis and treat with broad spectrum anti-infective (often also inducing adverse effects).
Pre-pubescent girls may also have infectious vaginitis, although the causes are different than those for women:
- Bacterial vaginosis: vaginitis caused by Streptococcus spp..
- Improper hygiene, which may introduce bacteria or other irritants from the anal region to the vaginal area.
The pH balance in adolescent girls' bodies is not conducive to the growth of Candida albicans, so they are unlikely to contract a yeast infection.
[edit]Hormonal
Hormonal vaginitis includes atrophic vaginitis usually found in postmenopausal or postpartum women. Sometimes it can occur in young girls before puberty. In these situations the estrogen support of the vagina is poor.
[edit]Irritation/allergy
Irritant vaginitis can be caused by allergies to condoms, spermicides, soaps, perfumes, douches, lubricants and semen. It can also be caused by hot tubs, abrasion, tissue, tamponsor topical medications.
[edit]Foreign body
Foreign Body Vaginitis: Foreign bodies (most commonly retained tampons or condoms) cause extremely malodorous vaginal discharges. Treatment consists of removal, for which ring forceps may be useful. Further treatment is generally not necessary.
[edit]Role of STDs
Sexually Transmitted Diseases (STDs) can be a cause of vaginal discharge. Chlamydia and gonorrhea testing should be done whenever a sexually active individual complains of vaginal discharge even when the cervix appears normal.
[edit]Diabetes
[edit]Diagnosis
Diagnosis is made with microscopy (mostly by vaginal wet mount) and culture of the discharge after a careful history and physical examination have been completed. The color, consistency, acidity, and other characteristics of the discharge may be predictive of the causative agent. The International Statistical Classification of Diseases and Related Health Problems codes for the several causes of vaginitis are:
| Condition | Description | pH |
|---|---|---|
| Candida vaginitis(B37.3) | Commonly referred to as a yeast infection, Candidiasis is a fungal infection that usually causes a watery, white, cottage cheese like vaginal discharges. The discharge is irritating to the vagina and the surrounding skin. | low (4.0-4.5) |
| Atrophic vaginitis(or Senile vaginitis) (N95.2) | usually causes scant vaginal discharge with no odour, dry vagina and painful intercourse. These symptoms are usually due to decreased hormones usually occurring during and after menopause. | |
| Bacterial vaginitis(B96.3). | Gardnerella usually causes a discharge with a fish-like odour. It is associated with itching and irritation, but not pain during intercourse. | elevated |
| Trichomonas vaginalis(A59.0) | can cause a profuse discharge with a fish-like odour, pain upon urination, painful intercourse, and inflammation of the external genitals. | elevated (5.0-6.0) |
| Herpes(A60.0) | usually occurs as water blisters on the genital region, about one week after infection. There is tenderness, swollen glands, and fever. The water blisters are extremely painful and heal in about three weeks. However, herpes is usually an external infection and does not fall under the category of vaginitis. |
[edit]Complications
- persistent discomfort
- superficial skin infection (from scratching)
- complications of the causative condition (such as gonorrhea and candida infection)
[edit]Treatment
The cause of the infection determines the appropriate treatment. It may include oral or topical antibiotics and/or antifungal creams, antibacterial creams, or similar medications. A cream containing cortisone may also be used to relieve some of the irritation. If an allergic reaction is involved, an antihistamine may also be prescribed. For women who have irritation and inflammation caused by low levels of estrogen (postmenopausal), a topical estrogen cream might be prescribed.
Often, after an anti-infective treatment, the vaginal flora (aka Döderlein flora) is disturbed. The cause is the reduced density of live flora (physiological barrier against pathogens) and the reduction of the vaginal epithelium (physical barrier against pathogens). As a result, post antiinfective treatment also requests the strengthening of the natural vaginal flora, which is done with local administration of lactobacillus and potentially low dose of hormone (e.g. estriol) to increase the proliferation of the epithelial cells. [6]
Fallopian tube
Fallopian tube
From Wikipedia, the free encyclopedia
| It has been suggested that Oviduct be merged into this article or section. (Discuss) |
| Fallopian tube | |
|---|---|
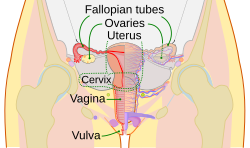 | |
| Schematic frontal view of female anatomy | |
 | |
| Vessels of the uterus and its appendages, rear view. (Fallopian tubes visible at top right and top left.) | |
| Latin | tuba uterina |
| Gray's | subject #267 1257 |
| Artery | tubal branches of ovarian artery, tubal branch of uterine artery |
| Lymph | lumbar lymph nodes |
| Precursor | Müllerian duct |
| MeSH | Fallopian+Tubes |
The Fallopian tubes, named after Gabriel Fallopius (Gabriele Falloppio), also known asoviducts, uterine tubes, and salpinges (singular salpinx) are two very fine tubes lined withciliated epithelia, leading from the ovaries of female mammals into the uterus, via the utero-tubal junction. In non-mammalian vertebrates, the equivalent structures are the oviducts.
Contents[hide] |
[edit]Anatomy and histology
The tube connects the ovary to the uterus as the egg passes through it in a woman's body. Its different segments are (lateral to medial): the infundibulum with its associated fimbriae near the ovary, the ampullary region that represents the major portion of the lateral tube, theisthmus which is the narrower part of the tube that links to the uterus, and the interstitial (also intramural) part that transverses the uterine musculature. The tubal ostium is the point where the tubal canal meets the peritoneal cavity, while the uterine opening of the Fallopian tube is the entrance into the uterine cavity, the utero-tubal junction.
There are two types of cells within the simple columnar epithelium of the Fallopian tube. Ciliated cells predominate throughout the tube, but are most numerous in the infundibulum and ampulla. Estrogen increases the production of cilia on these cells. Interspersed between the ciliated cells are peg cells, which contain apical granules and produce the tubular fluid. This fluid contains nutrients for spermatzoa, oocytes, and zygotes. The secretions also promote capacitation of the sperm by removing glycoproteins and other molecules from the plasma membrane of the sperm. Progesterone increases the number of peg cells, while estrogen increases their height and secretory activity. Tubal fluid flows against the action of the ciliae, that is toward the fimbrated end.
[edit]Function in fertilization
When an ovum is developing in an ovary, it is encapsulated in a sac known as an ovarian follicle. On maturity of the ovum, the follicle and the ovary's wall rupture, allowing the ovum to escape. The egg is caught by the fimbriated end and travels to the ampulla where typically the sperm are met and fertilization occurs; the fertilized ovum, now a zygote, travels towards the uterus aided by activity of tubal cilia and activity of the tubal muscle. After about five days the now embryo enters the uterine cavity and implants about a day later.
Occasionally the embryo implants into the Fallopian tube instead of the uterus, creating an ectopic pregnancy, commonly known as a "tubal pregnancy".
[edit]Patency testing
While a full testing of tubal functions in patients with infertility is not possible, tesing of tubal patency is important as tubal obstruction is a major cause of childlessness. A hysterosalpingogram will demonstrate that tubes are open when the radioopaque dye spills into the uterine cavity. Tubal insufflation is a office method to indicate patency. during surgery the status of the tubes can be inspected and a dye such asmethylene blue can be injected into the uterus and shown to pass through the tubes when the cervix is occluded.
[edit]Embryology and homology
Embryos have two pairs of ducts to let gametes out of the body; one pair (the Müllerian ducts) develops in females into the Fallopian tubes, uterus and vagina, while the other pair (the Wolffian ducts) develops in males into the epididymis and vas deferens.
Normally, only one of the pairs of tubes will develop while the other regresses and disappears in utero.
The homologous organ in the male is the rudimentary appendix testis.
[edit]Pathology
Pelvic inflammatory disease can strike the fallopian tubes. This might cause a Fallopian tube obstruction. Fallopian tube cancer is a rare neoplasm that can arise from the epithelial lining of the Fallopian tube. This cancer is sometimes misdiagnosed as ovarian cancer [1]. However, treatment of both ovarian and Fallopian tube cancer is similar.
[edit]Surgery
The surgical removal of a Fallopian tube is called a salpingectomy. To remove both sides is a bilateral salpingectomy. An operation that combines the removal of a Fallopian tube with removal of at least one ovary is a salpingo-oophorectomy. An operation to restore a fallopian tube obstruction is called a tuboplasty.
[edit]Etymology and nomenclature
They are named after their discoverer, the 16th century Italian anatomist, Gabriele Falloppio.
Though the name 'Fallopian tube' is eponymous, some texts spell it with a lower case 'f' from the assumption that the adjective 'fallopian' has been absorbed into modern English as the de facto name for the structure.
[edit]Additional images
[edit]
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||










No comments:
Post a Comment