 | |
|---|---|
| Systematic (IUPAC) name | |
| (6R,7R,Z)-3-(acetoxymethyl)-7-(2-(2-aminothiazol-4-yl)- 2-(methoxyimino)acetamido)-8-oxo-5-thia-1-azabicyclo[4.2.0] oct-2-ene-2-carboxylic acid | |
| Identifiers | |
| CAS number | 63527-52-6 |
| ATC code | J01DD01 |
| PubChem | CID 5479527 |
| DrugBank | APRD00854 |
| ChemSpider | 4586392 |
| Chemical data | |
| Formula | C16H17N5O7S2 |
| Mol. mass | 455.47 g/mol |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | n/a |
| Metabolism | Hepatic |
| Half-life | 0.8–1.4 hours |
| Excretion | 50–85% renal |
| Therapeutic considerations | |
| Pregnancy cat. | B1(AU) B(US) |
| Legal status | Prescription Only (S4) (AU) |
| Routes | Intravenous |
| | |
Cefotaxime (INN) (pronounced /ˌsɛfɵˈtæksiːm/) is a third-generation cephalosporinantibiotic. Like other third-generation cephalosporins, it has broad spectrum activity against Gram positive and Gram negative bacteria. In most cases, it is considered to be equivalent to ceftriaxone in terms of safety and efficacy. Cefotaxime sodium is marketed under various trade names including Kefotex® by Gepach International,CEfoTaX by EIPICO and Claforan by Roussel-Uclaf.
Contents[hide] |
[edit]Mechanism of action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.[1]
Cefotaxime, like other β-lactam antibiotics does not only block the division of bacteria, including cyanobacteria, but also the division of cyanelles, thephotosynthetic organelles of the Glaucophytes, and the division of chloroplasts ofbryophytes. In contrast, it has no effect on the plastids of the highly developed vascular plants. This is supporting the endosymbiotic theory and indicates anevolution of plastid division in land plants [2].
[edit]Clinical use
Cefotaxime is used for infections of the respiratory tract, skin, bones, joints,urogenital system, meningitis, and septicemiagastrointeritis. It generally has good coverage against most Gram-negative bacteria, with the notable exception ofPseudomonas. It is also effective against most Gram-positive cocci except forEnterococcus.[1] It is active against penicillin-resistant strains of Streptococcus pneumoniae. It has modest activity against the anaerobic Bacteroides fragilis.
[edit]Chemistry
The syn-configuration of the methoxyimino moiety confers stability to β-lactamase enzymes produced by many Gram-negative bacteria. Such stability to β-lactamases increases the activity of cefotaxime against otherwise resistant Gram-negative organisms.
 | |
|---|---|
 | |
| Systematic (IUPAC) name | |
| (2S,5R,6R)-6-([(2R)-2-amino-2-phenylacetyl]amino) -3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2- carboxylic acid | |
| Identifiers | |
| CAS number | 69-53-4 |
| ATC code | J01CA01 S01AA19 QJ51CA01 |
| PubChem | CID 6249 |
| DrugBank | DB00415 |
| ChemSpider | 6013 |
| Chemical data | |
| Formula | C16H19N3O4S |
| Mol. mass | 349.41 g·mol−1 |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | 40% (oral) |
| Protein binding | 15 to 25% |
| Metabolism | 12 to 50% |
| Half-life | approx 1 hour |
| Excretion | 75 to 85% renal |
| Therapeutic considerations | |
| Pregnancy cat. | A (Au), B (U.S.) |
| Legal status | |
| Routes | Oral, intravenous |
| | |
Ampicillin is a beta-lactam antibiotic that has been used extensively to treat bacterial infectionssince 1961. Until the introduction of ampicillin by the British company Beecham, penicillin therapies had only been effective against Gram-positive organisms such as staphylococci andstreptococci. Ampicillin (originally branded as 'Penbritin') also demonstrated activity againstGram-negative organisms such as H. influenzae, coliforms and Proteus spp. Ampicillin was the first of a number of so-called broad spectrum penicillins subsequently introduced by Beecham. Ampicillin is part of the aminopenicillin family and is roughly equivalent to its successor,amoxicillin in terms of spectrum and level of activity[1]. It can sometimes result in reactions that range in severity from a rash (in the case of patients that may unwittingly have mononucleosis) to potentially lethal allergic reactions such as anaphylaxis. However, as with other penicillin drugs, it is relatively non-toxic and adverse effects of a serious nature are encountered only infrequently.
Contents[hide] |
[edit]Mechanism of action
Belonging to the penicillin group of beta-lactam antibiotics, ampicillin is able to penetrate Gram-positive and some Gram-negative bacteria. It differs from penicillin only by the presence of anamino group. That amino group helps the drug penetrate the outer membrane of gram-negative bacteria.
Ampicillin acts as a competitive inhibitor of the enzyme transpeptidase, which is needed by bacteria to make their cell walls.[1] It inhibits the third and final stage of bacterial cell wall synthesis in binary fission, which ultimately leads to cell lysis.The holes that appear in the cell walls allow the body’s immune system to take over and fight off the bacteria. Ampicillin has received FDA approval for its action of mechanism.
[edit]Effects on chloroplast division
Ampicillin, like other β-lactam antibiotics, not only blocks the division of bacteria, but also the division of chloroplasts of the Glaucophytes (called cyanelles) and chloroplasts of the mossPhyscomitrella patens, a bryophyte. In contrast, it has no effect on the plastids of the higher developed vascular plant Lycopersicon esculentum L. (tomato) [2].
[edit]Application
Ampicillin is closely related to amoxicillin, another type of penicillin, and both are used to treaturinary tract infections, otitis media, uncomplicated community-acquired pneumonia,Haemophilus influenzae, salmonellosis and Listeria meningitis. It is used with flucloxacillin in the combination antibiotic co-fluampicil forempiric treatment of cellulitis; providing cover against Group A streptococcal infection whilst the flucloxacillin acts against the Staphylococcus aureus bacterium. Of concern is the number of bacteria that become resistant to Ampicillin necessitating combination therapy or use of otherantibiotics.
[edit]Use in research
Ampicillin is often used as a selective agent in molecular biology to select for and to confirm the uptake of genes (e.g., of plasmids) by bacteria (e.g., E. coli). A gene that is to be inserted into a bacterium is coupled to a gene coding for an ampicillin resistance (in E. coli, usually the bla (TEM-1) gene, coding for β-lactamase). The treated bacteria are then grown in a medium containing ampicillin (typically 50–100 mg/L). Only the bacteria that successfully take up the desired genes become ampicillin resistant, and therefore contain the other desired gene as well. It can be used with Cloaxicillin as well. As a powder ampicillin is white with slight yellow cast and is soluble in water (150 mg/ml).
 | |
|---|---|
 | |
| Systematic (IUPAC) name | |
| 2,2-dichloro-N-[(1R,2R)-2-hydroxy-1-(hydroxymethyl)-2-(4-nitrophenyl)ethyl]acetamide | |
| Identifiers | |
| CAS number | 56-75-7 |
| ATC code | D06AX02 D10AF03 G01AA05J01BA01 S01AA01 S02AA01S03AA08 QJ51BA01 |
| PubChem | CID 298 |
| DrugBank | DB00446 |
| ChemSpider | 5744 |
| Chemical data | |
| Formula | C11H12Cl2N2O5 |
| Mol. mass | 323.132 g/mol |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | 75–90% |
| Metabolism | Hepatic |
| Half-life | 1.5–4.0 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | C (systemic), A (topical) |
| Legal status | Ocular P, else POM (UK) |
| Routes | Topical (ocular), oral, IV, IM |
| | |
Chloramphenicol (INN) is a bacteriocidal antimicrobial. It is considered a prototypical broad-spectrum antibiotic, alongside the tetracyclines.
Chloramphenicol is effective against a wide variety of Gram-positive and Gram-negative bacteria, including most anaerobic organisms. Due to resistance and safety concerns, it is no longer afirst-line agent for any indication in developed nations, although it is sometimes used topically foreye infections; nevertheless, the global problem of advancing bacterial resistance to newer drugs has led to renewed interest in its use.[1] In low-income countries, chloramphenicol is still widely used because it is exceedingly inexpensive and readily available.
The most serious adverse effect associated with chloramphenicol treatment is bone marrowtoxicity, which may occur in two distinct forms: bone marrow suppression, which is a direct toxic effect of the drug and is usually reversible, and aplastic anemia, which is idiosyncratic (rare, unpredictable, and unrelated to dose) and generally fatal.[2]
Contents[hide] |
[edit]Spectrum of activity
Because it functions by inhibiting bacterial protein synthesis, chloramphenicol has a very broad spectrum of activity: it is active against Gram-positive bacteria (including most strains of MRSA),Gram-negative bacteria and anaerobes.[3] It is not active against Pseudomonas aeruginosa,Chlamydiae, or Enterobacter species. It has some activity against Burkholderia pseudomallei, but is no longer routinely used to treat infections caused by this organism (it has been superseded by ceftazidime and meropenem). In the West, chloramphenicol is mostly restricted to topical uses because of the worries about the risk of aplastic anaemia.
[edit]Therapeutic uses
The original indication of chloramphenicol was in the treatment of typhoid, but the now almost universal presence of multi-drug resistantSalmonella typhi has meant that it is seldom used for this indication except when the organism is known to be sensitive. Chloramphenicol may be used as a second-line agent in the treatment of tetracycline-resistant cholera.
Because of its excellent BBB penetration (far superior to any of the cephalosporins), chloramphenicol remains the first choice treatment forstaphylococcal brain abscesses. It is also useful in the treatment of brain abscesses due to mixed organisms or when the causative organism is not known.
Chloramphenicol is active against the three main bacterial causes of meningitis: Neisseria meningitidis, Streptococcus pneumoniae andHaemophilus influenzae. In the West, chloramphenicol remains the drug of choice in the treatment of meningitis in patients with severepenicillin or cephalosporin allergy and GPs are recommended to carry intravenous chloramphenicol in their bag. In low income countries, the WHO recommend that oily chloramphenicol be used first-line to treat meningitis.
Chloramphenicol has been used in the U.S. in the initial empirical treatment of children with fever and a petechial rash, when the differential diagnosis includes both Neisseria meningitidis septicaemia as well as Rocky Mountain spotted fever, pending the results of diagnostic investigations.
Chloramphenicol is also effective against Enterococcus faecium, which has led to it being considered for treatment of vancomycin-resistant enterococcus.
Although unpublished, recent research suggests that chloramphenicol could also be applied to frogs to prevent their widespread destruction from fungal infections.[4]
Chloramphenicol has recently been discovered to be a life saving cure for chytridiomycosis in amphibians.[5] Chytridiomycosis is a fungal disease, blamed for the extinction of one-third of the 120 frog species lost since 1980.
[edit]Adverse effects
[edit]Aplastic anemia
The most serious side effect of chloramphenicol treatment is aplastic anaemia.[2] This effect is rare and is generally fatal: there is no treatment and there is no way of predicting who may or may not get this side effect. The effect usually occurs weeks or months after chloramphenicol treatment has been stopped and there may be a genetic predisposition.[6] It is not known whether monitoring the blood counts of patients can prevent the development of aplastic anaemia, but it is recommended that patients have a blood count checked twice weekly while on treatment. The highest risk is with oral chloramphenicol[7] (affecting 1 in 24,000–40,000)[8] and the lowest risk occurs with eye drops (affecting less than 1 in 224,716 prescriptions).[9]
Thiamphenicol is a related compound with a similar spectrum of activity that is available in Italy and China for human use, and has never been associated with aplastic anaemia[citation needed]. Thiamphenicol is available in the U.S. and Europe as a veterinary antibiotic, and is not approved for use in humans.
[edit]Bone marrow suppression
It is common for chloramphenicol to cause bone marrow suppression during treatment: this is a direct toxic effect of the drug on humanmitochondria. This effect manifests first as a fall in hemoglobin levels and occurs quite predictably once a cumulative dose of 20 g has been given. This effect is fully reversible once the drug is stopped and does not predict future development of aplastic anaemia.
[edit]Leukemia
There is an increased risk of childhood leukemia as demonstrated in a Chinese case-controlled study,[10] and the risk increases with length of treatment.
Possible Related Adverse Effects Chloramphenicol is particularly toxic to people sensitive to benzene based preservatives like preservatives 210 and 211. Chloramphenicol poisoning can cause sensitivity reactions to organic acids and salicylates. Chloramphenicol is also known to cause tinnitus and balance problems through inner ear damage. It also causes folic acid depletion resulting in adverse effects to the thyroid, pituitary and prostate through effects on PABA levels. There may also be links to chronic lymphocytic leukemia(CLL) through folic acid "depletion" and resultant high levels of folic acid in the mutant lymphocytes that characterize CLL Chloramphenicol stops the bodies production of vitamin D and pregnenolone. This results in major hormone depletion, including DHEA and testosterone, that can result in death and also lowers the bodies resistance to viral infection. Chloramphenicol can cause testes pain, possibly through hormone effects. Chinese research shows that chloramphenicol affects motor neurones. It also affects insulin Igf1 levels and glutamate levels. Both of these conditions are considered indicative of a type of motor neurone disease. The adverse genetic effects of chloramphenicol are considered heritable.
[edit]Gray baby syndrome
Intravenous chloramphenicol use has been associated with the so called gray baby syndrome.[11] This phenomenon occurs in newborn infants because they do not yet have fully functional liver enzymes (i.e. UDP-glucuronyl transferase), and so chloramphenicol remains unmetabolized in the body.[12] This causes several adverse effects, including hypotension and cyanosis. The condition can be prevented by using chloramphenicol at the recommended doses and monitoring blood levels.[13][14][15]
[edit]Pharmacokinetics
Chloramphenicol is extremely lipid soluble, it remains relatively unbound to protein and is a small molecule: it has a large apparent volume of distribution of 100 litres and penetrates effectively into all tissues of the body, including the brain. The concentration achieved in brain andcerebrospinal fluid (CSF) is around 30 to 50% even when the meninges are not inflamed; this increases to as high as 89% when the meninges are inflamed.
[edit]Use in special populations
Chloramphenicol is metabolised by the liver to chloramphenicol glucuronate (which is inactive). In liver impairment, the dose of chloramphenicol must therefore be reduced. There is no standard dose reduction for chloramphenicol in liver impairment, and the dose should be adjusted according to measured plasma concentrations. Chloramphenicol is also noted for its cause of "Gray Baby Syndrome" because of infants lack of the enzyme glucoronyl transferase which is the main pathway conjugational excretion, which leads to a buildup of the chemical in infants system- contraindication.[citation needed]
The majority of the chloramphenicol dose is excreted by the kidneys as the inactive metabolite, chloramphenicol glucuronate. Only a tiny fraction of the chloramphenicol is excreted by the kidneys unchanged. It is suggested that plasma levels be monitored in patients with renal impairment, but this is not mandatory. Chloramphenicol succinate ester (the inactive intravenous form of the drug) is readily excreted unchanged by the kidneys, more so than chloramphenicol base, and this is the major reason why levels of chloramphenicol in the blood are much lower when given intravenously than orally.[citation needed]
Chloramphenicol passes into breast milk and should therefore be avoided during breastfeeding if possible.[17]
[edit]Dose monitoring
Plasma levels of chloramphenicol must be monitored in neonates and in patients with abnormal liver function. It is recommended that plasma levels be monitored in all children under the age of 4, the elderly and patients with renal failure. Peak levels (1 hour after the dose is given) should be 15–25 mg/l; trough levels (taken immediately before a dose) should be less than 15 mg/l.[citation needed]
[edit]Drug interactions
Administration of chloramphenicol concomitantly with bone marrow depressant drugs is contraindicated, although concerns over aplastic anaemia associated with ocular chloramphenicol have largely been discounted.[18]
Chloramphenicol is a potent inhibitor of the cytochrome P450 isoforms CYP2C19 and CYP3A4 in the liver.[19] Inhibition of CYP2C19 causes decreased metabolism and therefore increased levels of, for example, antidepressants, antiepileptics and proton pump inhibitors if they are given concomitantly. Inhibition of CYP3A4 causes increased levels of, for example, calcium channel blockers, immunosuppressants,chemotherapeutic drugs, benzodiazepines, azole antifungals, tricyclic antidepressants, macrolide antibiotics, SSRIs, statins and PDE5 inhibitors.[20]
[edit]Mechanism of action
Chloramphenicol is bacteriostatic (that is, it stops bacterial growth). It is a protein synthesis inhibitor, inhibiting peptidyl transferase activity of the bacterial ribosome, binding to A2451 and A2452 residues in the 23S rRNA of the 50S ribosomal subunit, preventing peptide bond formation.[21] While chloramphenicol and the macrolide class of antibiotics both interact with ribosomes, chloramphenicol is not a macrolide. Chloramphenicol directly interferes with substrate binding, macrolides sterically block the progression of the growing peptide. [22] [23] [24]
[edit]Resistance
There are three mechanisms of resistance to chloramphenicol: reduced membrane permeability, mutation of the 50S ribosomal subunit and elaboration of chloramphenicol acetyltransferase. It is easy to select for reduced membrane permeability to chloramphenicol in vitro by serial passage of bacteria, and this is the most common mechanism of low-level chloramphenicol resistance. High-level resistance is conferred by the cat-gene; this gene codes for an enzyme called chloramphenicol acetyltransferase which inactivates chloramphenicol by covalently linking one or two acetyl groups, derived from acetyl-S-coenzyme A, to the hydroxyl groups on the chloramphenicol molecule. The acetylation prevents chloramphenicol from binding to the ribosome. Resistance-conferring mutations of the 50S ribosomal subunit are rare.
Chloramphenicol resistance may be carried on a plasmid that also codes for resistance to other drugs. One example is the ACCoT plasmid (A=ampicillin, C=chloramphenicol, Co=co-trimoxazole, T=tetracycline) which mediates multi-drug resistance in typhoid (also called R factors).
[edit]Formulations
Chloramphenicol is available as 250 mg capsules or as a liquid (125 mg/5 ml). In some countries, chloramphenicol is sold as chloramphenicol palmitate ester. Chloramphenicol palmitate ester is inactive, and is hydrolysed to active chloramphenicol in the small intestine. There is no difference in bioavailability between chloramphenicol and chloramphenicol palmitate.
The intravenous (IV) preparation of chloramphenicol is the succinate ester, because pure chloramphenicol does not dissolve in water. This creates a problem: chloramphenicol succinate ester is an inactive prodrug and must first be hydrolysed to chloramphenicol; the hydrolysis process is incomplete and 30% of the dose is lost unchanged in the urine, therefore serum concentrations of chloramphenicol are only 70% of those achieved when chloramphenicol is given orally.[25] For this reason, the chloramphenicol dose needs to be increased to 75 mg/kg/day when administered IV in order to achieve levels equivalent to the oral dose.[26] The oral route is therefore preferred to the intravenous route.
Manufacture of oral chloramphenicol in the U.S. stopped in 1991, because the vast majority of chloramphenicol-associated cases of aplastic anaemia are associated with the oral preparation. There is now no oral formulation of chloramphenicol available in the U.S.
[edit]Oily
Dose: 100 mg/kg (maximum dose 3 g) as a single intramuscular injection. The dose is repeated if there is no clinical response after 48 hours. A single injection costs approximately US$5.
Oily chloramphenicol (or chloramphenicol oil suspension) is a long-acting preparation of chloramphenicol first introduced by Roussel in 1954; marketed as Tifomycine, it was originally used as a treatment for typhoid. Roussel stopped production of oily chloramphenicol in 1995; theInternational Dispensary Association has manufactured it since 1998, first in Malta and then in India from December 2004.[citation needed]
Oily chloramphenicol is recommended by the World Health Organization (WHO) as the first line treatment of meningitis in low-income countries and appears on the essential drugs list. It was first used to treat meningitis in 1975[27] and there have been numerous studies since demonstrating its efficacy.[28][29][30] It is the cheapest treatment available for meningitis (US$5 per treatment course, compared to US$30 forampicillin and US$15 for five days of ceftriaxone). It has the great advantage of requiring only a single injection, whereas ceftriaxone is traditionally given daily for five days. This recommendation may yet change now that a single dose of ceftriaxone (cost US$3) has been shown to be equivalent to one dose of oily chloramphenicol.[31]
Oily chloramphenicol is not currently available in the U.S. or Europe.
[edit]Eye drops
In the West, chloramphenicol is still widely used in topical preparations (ointments and eye drops) for the treatment of bacterial conjunctivitis. Isolated cases report of aplastic anaemia following chloramphenicol eyedrops exist, but the risk is estimated to be less than 1 in 224,716 prescriptions.[9] Note. http://www.patient.co.uk/showdoc/40025037/ suggests that the link between chloramphenicol eye drops and aplastic anemia is "not well founded".
[edit]Trade names
Chloramphenicol has a long history and therefore a multitude of alternative names in many different countries:
- Alficetyn
- Amphicol
- Biomicin
- Chlornitromycin
- Chloromycetin (U.S., intravenous preparation)
- Chlorsig (U.S., Australia, eye drops)
- Dispersadron C (Greece, eye drops)
- Edrumycetin 250 mg (Bangladesh, Capsule)
- Fenicol
- Kemicetine (UK, intravenous preparation)
- Kloramfenikol (Denmark, eye drops)
- Laevomycetin
- UK as an eye treatment
- Brochlor (Aventis Pharma Ltd)
- Chloromycetin Redidrops (Goldshield Pharmaceuticals Ltd)
- Golden Eye (Typharm Ltd)
- Optrex Infected Eyes
- Oftan Chlora (eye ointment)
- Optacloran (Bolivia, eye drops)
- Phenicol
- Posifenicol 1% (Germany, eye ointment)
- Medicom
- Nevimycin
- Renicol (India,eye drops)
- Silmycetin (Thailand, eye drops)
- Synthomycine (Israel, eye ointment and skin ointment)
- Tifomycine (France, oily chloramphenicol)
- Vernacetin
- Veticol
- Orchadexoline (Egypt , eye drops)
- Isoptophenicol (Egypt . eye drops)
- Cedoctine (Egypt .intravenous preparation)
- Chloramex (South Africa, eye ointment)
[edit]History
Chloramphenicol was originally derived from the bacterium Streptomyces venezuelae, isolated by David Gottlieb, and introduced into clinical practice in 1949, under the trade name Chloromycetin. It was the first antibiotic to be manufactured synthetically on a large scale.
Co-trimoxazole
 | |
|---|---|
| Combination of | |
| Trimethoprim | Dihydrofolate reductaseinhibitor (16.7%) |
| Sulfamethoxazole | Sulfonamide antibiotic(83.3%) |
| Identifiers | |
| CAS number | 8064-90-2 |
| ATC code | J01EE01 |
| PubChem | CID 358641 |
| ChemSpider | 318412 |
| Therapeutic considerations | |
| Pregnancy cat. | C(AU) C(US) |
| Legal status | ℞-only (US) |
| Routes | Oral |
Co-trimoxazole (abbreviated SXT, TMP-SMX, TMP-SMZ or TMP-sulfa) is a sulfonamideantibiotic combination of trimethoprim and sulfamethoxazole, in the ratio of 1 to 5, used in the treatment of a variety of bacterial infections. The name co-trimoxazole is the British Approved Name, and has been marketed worldwide under many trade names including Septra (GSK),Bactrim (Roche), and various generic preparations. Sources differ as to whether co-trimoxazole usually is bactericidal or bacteriostatic.
Contents[hide] |
[edit]Synergistic action
The synergy between trimethoprim and sulphamethoxazole was first described in a series of in vitro and in vivo experiments published in the late 1960s.[1][2][3] Trimethoprim and sulfamethoxazole have a greater effect when given together than when given separately; the reason is because they inhibit successive steps in the folate synthesis pathway (see diagram below).
It is unclear whether this synergy occurs at doses used in humans,[4] because at the concentrations seen in blood and tissues, the ratio of trimethoprim to sulphamethoxazole is 1:20,[5] which is less than the 1:5 ratio needed in vitro for synergy to occur.
Sulfamethoxazole acts as a false-substrate inhibitor of dihydropteroate synthetase. Sulfonamides such as sulfamethoxazole are analogues ofp-aminobenzoic acid (PABA) and are competitive inhibitors of the enzyme; inhibiting the production of dihydropteroic acid.
Trimethoprim acts by interfering with the action of bacterial dihydrofolate reductase, inhibiting synthesis of tetrahydrofolic acid.
Folic acid is an essential precursor in the de novo synthesis of the DNA nucleosides thymidine and uridine. Bacteria are unable to take up folic acid from the environment (i.e. the infection host) thus are dependent on their own de novo synthesis - inhibition of the enzyme starves the bacteria of two bases necessary for DNA replication and transcription.
[edit]Clinical indications
Co-trimoxazole was claimed to be more effective than either of its components individually in treating bacterial infections, although this was later disputed.[6] Along with its associated greater incidence of adverse effects including allergic responses (see below), its widespread use has been restricted in many countries to very specific circumstances where its improved efficacy is demonstrated.[7] It may be effective in a variety of upper and lower respiratory tract infections, renal and urinary tract infections, gastrointestinal tract infections, skin and wound infections, septicaemias and other infections caused by sensitive organisms. The global problem of advancing antimicrobial resistance has led to a renewed interest in the use of co-trimoxazole in various settings more recently.[8]
Specific indications for its use include:
[edit]HIV
Being an antibiotic, co-trimoxazole does not have any activity against HIV itself, but it is often prescribed to immunocompromised patients asPneumocystis carinii pneumonia prophylaxis.
Also this antibiotic reduces the incidence of malaria by a 25% percent[Citation needed].
[edit]Bacterial
- infections caused by Listeria monocytogenes, Nocardia spp., Stenotrophomonas maltophilia (Zanthomonas maltophilia)
- Staphylococcus saprophyticus infections presenting as urinary tract infection or cystitis
- melioidosis
- shigellosis
- Whipple's disease
- traveller's diarrhea
[edit]Protozoan
- Isosporiasis[9]
- prophylaxis of cerebral toxoplasmosis in HIV patients
[edit]Fungal
- treatment and prophylaxis of pneumonia caused by Pneumocystis jirovecii (formerly identified as P. carinii and commonly seen in immunocompromised patients including those suffering from HIV/AIDS)
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed.(September 2008) |
[edit]Safety
There has been some concern about its use, however, since it has been associated with both frequent mild allergic reactions and serious adverse effects including Stevens-Johnson syndrome, myelosuppression, mydriasis, agranulocytosis, as well as severe liver damage (cholestatic hepatosis, hepatitis, liver necrosis, fulminant liver failure).[citation needed] Due to displacement of bilirubin from albumin there is an increased risk of kernicterus in the newborn during the last 6 weeks of pregnancy. Also renal impairment up to acute renal failure and anuria have been reported. These side effects are seen especially in the elderly and may be fatal. (Joint Formulary Committee, 2004). Folic acid is likely not the best option for the treatment of some adverse effects associated with TMP-SMX; a better treatment is probably administration offolinic acid.[clarification needed]
In some countries, co-trimoxazole has been withdrawn due to these toxic effects.[citation needed]
Thus the current British Committee on Safety of Medicines (CSM) guidelines recommend limiting its use to:[citation needed]
- Pneumocystis pneumonia
- Toxoplasmosis and nocardiosis
- acute exacerbations of chronic bronchitis and infections of the urinary tract where there is good rationale for use
- acute otitis media in children where there is good rationale
[edit]Trade names
Co-trimoxazole is manufactured and sold by many different companies. Some of the brand names are listed here, but this list is not complete.
- Bactrim®, Bactrimel® (Roche)
- Cotrim®
- Septrin®, Septra® (GlaxoSmithKline and formerly Burroughs Wellcome)
- Sulfatrim®
- Biseptol
Amoxicillin
| This article includes a list of references, related reading or external links, but its sources remain unclear because it lacks inline citations. Please improve this article by introducing more precise citationswhere appropriate. (August 2009) |
| ||||||||||||||||||||||||||||||||||||||||||||||||
Amoxicillin (INN), formerly amoxycillin (BAN), amoxycillin (cilamox) in Australia[1], abbreviated Amox,Tormoxin (in India), is a moderate-spectrum, bacteriolytic, β-lactamantibiotic used to treat bacterial infections caused by susceptible microorganisms. It is usually the drug of choice within the class because it is better absorbed, following oral administration, than other β-lactam antibiotics. It is also a treatment for cystic acne.[2]
Amoxicillin is susceptible to degradation by β-lactamase-producing bacteria, and so may be given with clavulanic acid to decrease its susceptibility.
Contents[hide] |
[edit]Mode of action
Main article: Beta-lactam antibiotic
Amoxicillin acts by inhibiting the synthesis of bacterial cell wall. It inhibits cross-linkagebetween the linear peptidoglycan polymer chains that make up a major component of the cell walls of both Gram-positive and Gram-negative bacteria
[edit]Formulations
Amoxicillin in trihydrate form is available as capsules, chewable and dispersible tablets plus syrup and pediatric suspension for oral use, and as the sodium salt for intravenousadministration (although the IV formulation is not available in the United States[3]). It is one of the most common antibiotics prescribed for children, and the liquid forms are helpful where the patient might find it difficult to take tablets or capsules. It has three ionizable groups. A once daily dosing form (Moxatag) was approved by the American FDA in January 2008.
[edit]Side effects
Side effects are as those for other beta-lactam antibiotics. Side effects include nausea, vomiting, rashes, and antibiotic-associated colitis. Loose bowel movements (diarrhea) also may occur. Rarer but patient reported side effects include mental changes, lightheadedness, confusion, suicidal thoughts, depression, anxiety, sensitivity to lights and sounds, unclear thinking. Immediate medical care is required upon the first signs of these side effects.
The onset of an allergic reaction to amoxicillin can be very sudden and intense - emergency medical attention must be sought as quickly as possible. The initial onset of such a reaction often starts with a change in mental state; skin rash with intense itching (often beginning in fingertips and around groin area and rapidly spreading) and sensations of fever, nausea, and vomiting. Any other symptoms that seem even remotely suspicious must be taken very seriously.
Use of the amoxicillin/clavulanic acid combination for more than one week has caused moderate to severe hepatitis in a number of patients. Young children who ingested acute overdoses of amoxicillin manifested lethargy, vomiting and renal dysfunction.[4][5]
[edit]Non-allergic amoxicillin rash
Somewhere between 3% to 10% of children taking amoxicillin (or ampicillin) show a late-developing (>72 hours after beginning medication and having never taken penicillin-like medication previously) often itchy rash [2][3], which is sometimes referred to as the "amoxicillin rash." The rash can also occur in adults.
The rash is described as maculopapular or morbilliform (measles-like; therefore, in medical literature, "amoxicillin-induced morbilliform rash"[6]). It starts on the trunk and can spread from there. This rash is unlikely to be a true allergic reaction, and is not a contra-indication for future amoxicillin usage, nor should current regimen necessarily be stopped. However, as mentioned above, this common amoxicillin rash and a dangerous allergic reaction cannot easily be distinguished by inexperienced persons, and therefore a health professional should be consulted if a rash develops. (Pichichero, 2005; Schmitt 2005)
A non-allergic amoxicillin rash may also be an indicator of infectious mononucleosis: Some studies indicate that approximately 80-90% of patients with acute Epstein Barr virus infection treated with amoxicillin or ampicillin develop such a rash.[7]
[edit]Proprietary preparations
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged andremoved. (February 2010) |
Amoxicillin is one of the semi-synthetic penicillins discovered by Beecham scientists. The patent for amoxicillin has expired, thus amoxicillin is marketed under many trade names, including:', Actimoxi, Alphamox, Amocla, AMK, Amoksibos, Amoxiclav Sandoz, Amoxidal, Amoxil, Amoxin, Amoksiklav, Amoxibiotic, Amoxicilina, Apo-Amoxi, Augmentin (with clavulanic acid), Bactox, Betalaktam, Cilamox, Curam, Dedoxil, Dispermox, Duomox, E-Mox, Enhancin, Gimalxina, Geramox, Hiconcil, Isimoxin, Klavox, Lamoxy, Moxatag, Moxilen, Moxypen, Moxyvit, Nobactam, Novamoxin, Ospamox, Panklav, Pamoxicillin, Panamox, Polymox, Samthongcillin, Clamoxyl, Senox, Sinacilin, Trimox, Tolodina, Tormoxin (India), Wymox, Yucla, Zerrsox and Zimox.
Streptomycin
 | |
|---|---|
 | |
| Systematic (IUPAC) name | |
| 5-(2,4-diguanidino- 3,5,6-trihydroxy-cyclohexoxy)- 4-[4,5-dihydroxy-6-(hydroxymethyl) -3-methylamino-tetrahydropyran-2-yl] oxy-3-hydroxy-2-methyl -tetrahydrofuran-3-carbaldehyde | |
| Identifiers | |
| CAS number | 57-92-1 |
| ATC code | A07AA04 J01GA01 |
| PubChem | CID 5999 |
| DrugBank | DB01082 |
| ChemSpider | 18508 |
| Chemical data | |
| Formula | C21H39N7O12 |
| Mol. mass | 581.574 g/mol |
| Physical data | |
| Melt. point | 12 °C (54 °F) |
| Pharmacokinetic data | |
| Bioavailability | 84% to 88% (est.)[1] |
| Half-life | 5 to 6 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | DM[2] |
| Legal status | POM (UK) ℞-only (US) |
| Routes | Intramuscular, intravenous |
Streptomycin is an antibiotic drug, the first of a class of drugs called aminoglycosides to be discovered, and was the first antibiotic remedy for tuberculosis. It is derived from theactinobacterium Streptomyces griseus. Streptomycin is a bactericidal antibiotic[3]. Streptomycin cannot be given orally, but must be administered by regular intramuscular injections. An adverse effect of this medicine is ototoxicity, which can lead to hearing loss[citation needed].
Contents[hide] |
[edit]Mechanism of action
Streptomycin is a protein synthesis inhibitor. It binds to the S12 Protein of the 30S subunit of the bacterial ribosome, interfering with the binding of formyl-methionyl-tRNA to the 30S subunit[4]. This prevents initiation of protein synthesis and leads to death of microbial cells. Humans have structurally different ribosomes from bacteria, thereby allowing the selectivity of this antibiotic for bacteria. However at low concentrations Streptomycin only inhibits growth of the bacteria by inducing prokaryotic ribosomes to misread mRNA[5]. Streptomycin is an antibiotic that inhibits both gram positive and gram negative bacteria[citation needed], and is a therefore a useful broad spectrum antibiotic.
[edit]History
Streptomycin was first isolated on October 19, 1943 by Albert Schatz, a graduate student, in the laboratory of Selman Abraham Waksman at Rutgers University[6]. Waksman and his laboratory discovered several antibiotics, including actinomycin, clavacin, streptothricin, streptomycin,grisein, neomycin, fradicin, candicidin and candidin. Of these, streptomycin and neomycin found extensive application in the treatment of numerous infectious diseases. Streptomycin was the first antibiotic that could be used to cure the disease tuberculosis; early production of the drug was dominated by Merck & Co. under George W. Merck.
The first randomized trial of streptomycin against pulmonary tuberculosis was carried out in 1947 by the MRC Tuberculosis Research Unit. Whilst neither double-blind nor placebo-controlled, results showed efficacy against TB, albeit with minor toxicity and acquired bacterial resistanceto the drug.[7]
[edit]Uses
[edit]Treatment of diseases
- Tuberculosis in combination with other anti-TB drugs. It is not the first line treatment, except in medically under-served populations where the cost of more expensive treatments are prohibitive.
- Plague (Yersinia pestis) has historically been treated with it as the first line treatment. It is approved for this purpose by the U.S. Food and Drug Administration.
- Infective endocarditis caused by enterococcus when the organism is not sensitive to Gentamicin
- In veterinary medicine, streptomycin is the first line antibiotic for use against gram negative bacteria in large animals (horses, cattle, sheepetc.). It is commonly combined with procaine penicillin for intramuscular injection.
While streptomycin is traditionally given intramuscularly (indeed, in many countries it is only licensed to be used intramuscularly), the drug may also be administered intravenously.[1]
[edit]Pesticide
Streptomycin is also used as a pesticide, to combat the growth of bacteria, fungi, and algae. Streptomycin controls bacterial and fungal diseases of certain fruit, vegetables, seed, and ornamental crops, and controls algae in ornamental ponds and aquaria. A major use is in the control of fireblight on apple and pear trees. As in medical applications, extensive use can be associated with the development of resistant strains.
[edit]Cell Culture
Streptomycin, in combination with penicillin, is used in a standard antibiotic cocktail to prevent bacterial infection in cell culture.
Ciprofloxacin
"Cipro" redirects here. For the Rome Metro station, see Cipro (Rome Metro).
 | |
|---|---|
 | |
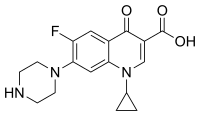
| Systematic (IUPAC) name | |
| 1-cyclopropyl- 6-fluoro- 4-oxo- 7-piperazin- 1-yl- quinoline- 3-carboxylic acid | |
| Identifiers | |
| CAS number | 85721-33-1 |
| ATC code | J01MA02 S01AX13 S02AA15S03AA07 |
| PubChem | CID 2764 |
| DrugBank | DB00537 |
| ChemSpider | 2662 |
| Chemical data | |
| Formula | C17H18FN3O3 |
| Mol. mass | 331.346 |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | 69%[1] |
| Metabolism | Hepatic, including CYP1A2 |
| Half-life | 4 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | B3(AU) C(US) |
| Legal status | Prescription Only (S4) (AU) POM(UK) |
| Routes | Oral, intravenous, topical (ear drops, eye drops) |
| | |
Ciprofloxacin (INN) is a synthetic chemotherapeutic antibiotic of the fluoroquinolone drug class.[2][3] It is a second-generation fluoroquinolone antibacterial. It kills bacteria by interfering with the enzymes that cause DNA to rewind after being copied, which stops DNA and protein synthesis.
Ciprofloxacin is marketed worldwide with over three hundred different brand names. In the United States, Canada, and the UK, it is marketed as Baycip, Ciloxan, Ciflox, Cipro, Cipro XR,Cipro XL, Ciproxin and most recently, Proquin. In Pakistan it is available under the brand name Starcip. In addition, ciprofloxacin is available as a generic drug under a variety of different brand names and is also available for limited use in veterinary medicine.
Ciprofloxacin was first patented in 1983 by Bayer A.G. and subsequently approved by the United States Food and Drug Administration (FDA) in 1987. Ciprofloxacin has 12 FDA-approved human uses and other veterinary uses, but it is often used for non-approved uses (off-label). Ciprofloxacin interacts with other drugs, herbal and natural supplements, and thyroid medications.[4]
[edit]History
The patent history for ciprofloxacin makes reference to a 1982 European Patent (patent number 0049355), as well a German patent dated 21 January 1986. Bayer introduced ciprofloxacin in 1987 and was later approved by the U.S. FDA on 22 October 22 1987 for use in the United States to treat specific bacterial infections. In 1991, the intravenous formulation was introduced. The current United States patent appears to be held by Bayer, being the assignee.[5] The United States patent was applied for in January 1987, but was not approved until 1996 according to the patent history.
In 2004, ciprofloxacin and levofloxacin together commanded 65% ($3.3 billion) of the global sales of the fluoroquinolone class.[6] The first nine months of 2008 sales for ciprofloxacin were $242 million, as compared to $324 million for Bayer aspirin.[7] Ciprofloxacin has proven to be a blockbuster drug for Bayer A. G., generating billions of dollars in additional revenue. "In 1999, Cipro was the eleventh most prescribed drug in the United States based on new prescriptions, and ranked twentieth in total United States sales. In 1999, Bayer's gross sales of Cipro in the United States were approximately $1.04 billion."[8] The sale of ciprofloxacin increased dramatically following the anthrax scare of 2001. On 24 October 2002, the Bush Administration (2001–2009) announced a deal between the government and Bayer Pharmaceuticals to purchase 100 million tablets of ciprofloxacin at a reduced price of $0.95 per pill. A full course of ciprofloxacin for postexposure prophylaxis (60 days) resulting from this arrangement costs the government $204 per person treated, compared with $12 per person treated with doxycycline, the drug normally used to treat anthrax, a difference of $192.[9]
- Generic equivalents:
On 24 October 2001, The Prescription Access Litigation (PAL), filed suit to dissolve an agreement between Bayer, Barr Laboratories, and two other generic drug companies that it claimed was blocking access to adequate supplies and cheaper, generic versions of ciprofloxacin. The plaintiffs charged that Bayer Corporation, a unit of Bayer AG, had unlawfully paid three of its competitors — Barr Laboratories, Rugby, and Hoechst-Marion Roussel — a total of $200 million to prevent cheaper, generic versions of ciprofloxacin from being brought to the market, as well as manipulating the price and supply of ciprofloxacin. Numerous other consumer advocacy groups joined this lawsuit. On 15 October 2008, five years after Bayer’s patent had expired, the United States District Court for the Eastern District of New York granted Bayer’s and the generic defendants’ motion for summary judgment, holding that any anticompetitive effects caused by the settlement agreements between Bayer and the generic defendants were within the exclusionary zone of the patent, and thus could not be redressed by federal antitrust law,[10] in effect upholding Bayer’s agreement to pay Barr Laboratories, Rugby, and Hoechst-Marion Roussel a total of $200 million to prevent the marketing a generic equivalent of ciprofloxacin.
[edit]Licensed uses
The licensed uses for ciprofloxacin in the United States are as follows:
In the adult population, ciprofloxacin is limited to the treatment of proven bacterial infections such as:
- Urinary tract infections (not recommended as a first-line antibiotic)[11]
- Acute uncomplicated cystitis in females
- Chronic bacterial prostatitis (not recommended as a first-line antibiotic choice)[12][13]
- Lower respiratory tract infections (not recommended as a first-line antibiotic choice)[14][15][16]
- Acute sinusitis (not recommended as a first-line antibiotic choice)[17]
- Skin and skin structure infections
- Bone and joint infections
- Infectious diarrhea
- Typhoid fever (enteric fever) caused by Salmonella typhi
- Uncomplicated cervical and urethra gonorrhea (due to N. gonorrhoeae) – however, this indication is no longer effective in some areas (e.g., Asian countries,[18] United States (including Hawaii), Canada ,[19] and Scotland)[20] due to bacterial resistance. Fluoroquinolones are no longer recommended in the USA for this indication.[21]
Ciprofloxacin is not recommended for the treatment of tuberculosis.[22]
As well as in combination with other specific drugs:
- Complicated intra-abdominal infections (in combination with metronidazole);
- Empirical therapy for febrile neutropenic patients (in combination with piperacillin)
Oral and intravenous fluoroquinolones are not licensed by the U.S. FDA for use in children due to the risk of permanent injury to the musculoskeletal system, with two exceptions as outlined below. Within the studies submitted in response to a Pediatric Written Request (Ciprofloxacin, circa 2004) the rate of arthropathy was reported to be 9.3% at one month and 13.6% at one year.[23] As such the pediatric use of ciprofloxacin is restricted to proven complicated urinary tract infections and pyelonephritis due to E. coli and inhalation anthrax.[24]Although claimed to be effective, ciprofloxacin is not to be considered a first line agent for inhalation anthrax in the pediatric population.[23][25][26][27] The CDC revoked its recommendation regarding the use of ciprofloxacin as a first line agent in treating anthrax due to the unacceptable risk documented within the Antimicrobial Postexposure Prophylaxis for Anthrax study (aka Cipro 60 day study).[28]However, the fluoroquinolones are licensed to treat lower respiratory infections in children with cystic fibrosis in the UK.
Current recommendations by the American Academy of Pediatrics note that the systemic use of ciprofloxacin in children should be restricted to infections caused by multidrug resistant pathogens or when no safe or effective alternatives are available.[29]
Indications include:
- Complicated urinary tract infections and pyelonephritis due to Escherichia coli[30]
Ciprofloxacin is not recommended to treat CAP (community acquired pneumonia) as a stand-alone first-line agent. The current guidelines (Infectious Diseases Society of America 2007) state that, in very limited circumstances, ciprofloxacin or levofloxacin should be combined with other drugs such as a b-lactam drug to treat specific CAP infections, but neither drug is recommended to be used separately as a stand-alone first-line agent. In addition, the current guidelines state that: “Data exist suggesting that resistance to macrolides and older fluoroquinolones (ciprofloxacin and levofloxacin) results in clinical failure. Other studies have shown that repeated use of fluoroquinolones predicts an increased risk of infection with fluoroquinolone-resistant pneumococci....”[32]
As such, the general opinion stated in 1994 that ciprofloxacin “is not to be considered a suitable agent for use in general practice for the blind initial treatment of chest infections....”[33][34] does not appear to have changed within these current guidelines.
Antibiotics may not improve the long-term clinical outcome for sinusitis.[35] When prescribed for chronic bronchitis and acute bacterial sinusitis, the use of the fluoroquinolone class offers no compelling advantages over established treatment.[36] Nor does antibiotic treatment help sore throats.[37] The use of antibiotics such as ciprofloxacin to treat bronchitis is to be considered unnecessary and as such exposes the patient to an unacceptable risk of suffering a severe adverse reaction.[38] Additionally, antibiotics have no effect upon viral infections, such as the common head cold or viral respiratory infections.
Note: Ciprofloxacin may be licensed for other uses, or restricted, by the various regulatory agencies worldwide.
[edit]Availability
Ciprofloxacin is available as:
- tablets (250 mg, 500 mg or 750 mg)
- intravenous solutions (5% and 10%, 100 mL)
- eye and ear drops
In most countries, all formulations require a prescription.
See the latest package insert for ciprofloxacin (Cipro) for additional details.[39]
[edit]Mode of action
Ciprofloxacin is a broad-spectrum antibiotic that is active against both Gram-positive and Gram-negative bacteria. It functions by inhibitingDNA gyrase, a type II topoisomerase, and topoisomerase IV,[40] enzymes necessary to separate bacterial DNA, thereby inhibiting cell division.
This mechanism can also affect mammalian cell replication. In particular, some congeners of this drug family (for example those that contain the C-8 fluorine)[41] display high activity not only against bacterial topoisomerases but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models.[42] Although quinolones are highly toxic to mammalian cells in culture, its mechanism of cytotoxic action is not known. Quinolone induced DNA damage was first reported in 1986 (Hussy et al.).[43]
Recent studies have demonstrated a correlation between mammalian cell cytotoxicity of the quinolones and the induction of micronuclei.[44][45][46][47] As such some fluoroquinolones may cause injury to the chromosome of eukaryotic cells.[48][49][50][51][52][53]
There continues to be debate as to whether or not this DNA damage is to be considered one of the mechanisms of action concerning the severe adverse reactions experienced by some patients following fluoroquinolone therapy.[42][54][55]
[edit]Contraindications
As noted above, under licensed use, ciprofloxacin is also now considered to be contraindicated for the treatment of certain sexually transmitted diseases by some experts due to bacterial resistance.[56]
There are only four contraindications found within the 2009 package insert:[39]
- “Coadministration of ciprofloxacin with other drugs primarily metabolized by CYP1A2 results in increased plasma concentrations of these drugs and could lead to clinically significant adverse events of the coadministered drug.”
- “Concomitant administration with tizanidine is contraindicated”
- “Ciprofloxacin is contraindicated in persons with a history of hypersensitivity to ciprofloxacin, any member of the quinolone class of antimicrobial agents, or any of the product components.”
- “Local I.V. site reactions are more frequent if the infusion time is 30 minutes or less. These may appear as local skin reactions that resolve rapidly upon completion of the infusion. Subsequent intravenous administration is not contraindicated unless the reactions recur or worsen.”'
Due to growing prevalence of antibiotic resistance to the fluoroquinolones in southeast Asia, the use of ciprofloxacin in patients having been to southeast Asia is increasingly being discouraged.[57]
Ciprofloxacin is also considered to be contraindicated within the pediatric population (except for the indications outlined under licensed use above), pregnancy, nursing mothers, and in patients with epilepsy or other seizure disorders.
- Pregnancy
The fluoroquinolones rapidly cross the blood-placenta and blood-milk barriers, and are extensively distributed into the fetal tissues. For this reason, the fluoroquinolones are contraindicated during pregnancy due to the risk of spontaneous abortions and birth defects. The fluoroquinolones have also been reported as being present in the mother’s milk and are passed on to the nursing child, which may increases the risk of the child suffering from this syndrome as well, even though the child had never been prescribed or taken any of the drugs found within this class.[58][59]
- Pediatric population
Fluoroquinolones are not licensed by the U.S. FDA for use in children due to the risk of fatalities[60] as well as permanent injury to the musculoskeletal system, with two exceptions. Ciprofloxacin is being licensed for the treatment of complicated urinary tract infections and pyelonephritis due to Escherichia coli, and inhalational anthrax (postexposure), and levofloxacin was recently licensed for the treatment of inhalational anthrax (postexposure). However, the fluoroquinolones are licensed to treat lower respiratory infections in children with cystic fibrosis in the UK.
Within the studies submitted in response to a Pediatric Written Request (Ciprofloxacin, circa 2004), the rate of atrophy was reported to be 9.3%.[61] Within the BPCA Pediatric Studies Summary for ciprofloxacin[61], it was stated that the overall incidence of adverse events at six weeks was 41%. This would be consistent with the safety profile found with the other fluoroquinolones studied in the pediatric population. As such, the current ban on the use of the fluoroquinolones in the pediatric population is both reasonable and supported by various clinical studies. The most recent long term study, BAY 0 9867 Cipro Pediatric Use Study (QUIP), which followed pediatric patients from 1999–2008,[62] supports the current expert opinion that the risk of permanent injury continues to outweigh the potential benefits of ciprofloxacin therapy in the pediatric population.
Within the United States, the FDA has stated it is their intention to pursue the licensing of the fluoroquinolones for pediatric use in spite of the evidence presented at that 62 Meeting of the Anti-Infective Drugs Advisory Committee that the fluoroquinolones cause irreversible joint damage in the pediatric population.[63]
- Depression and anxiety disorders
Ciprofloxacin has highly pronounced side effects in people suffering from panic disorder or/and depression. There have been reported cases of psychosis, suicide attempts, panic attacks and acute anxiety, all occurring during or shortly after ciprofloxacin treatment. Patients with previous or current psychiatric conditions, are prone to experiencing this type of side effect. Caution is highly advised.
[edit]Special precautions
The status of the patient’s renal function and hepatic function must also be taken into consideration to avoid an accumulation that may lead to an overdose and the development of toxicity. Ciprofloxacin is eliminated primarily by renal excretion. However, the drug is also metabolized and partially cleared through the liver and the intestine. Modification of the dosage is recommended using the table found within the package insert for those with impaired liver or kidney function. However, since the drug is known to be substantially excreted by the kidneys, the risk of toxic reactions to this drug may be greater in patients with impaired renal function. The duration of treatment depends upon the severity of infection and the usual duration is 7 to 14 days.[24]
[edit]Adverse effects
See also: Adverse effects of fluoroquinolones
Serious adverse events occur more commonly with fluoroquinolones than with any other antibiotic drug classes. In most, adverse reactions are mild to moderate; however, occasionally serious adverse effects occur.[64][65] There have been a number of regulatory actions taken as a result of such adverse reactions, which included published warnings,[66][67] additional warnings and safety information added to the package inserts[68] together with the issuance of "Dear Doctor Letters"[69] concerning the recent addition of Black Box Warnings. In 2004, the U.S. FDA requested new warning labels to be added to all of the fluoroquinolones, including ciprofloxacin, regarding peripheral neuropathy(irreversible nerve damage), tendon damage, heart problems (prolonged QT Interval / torsades de pointes), pseudomembranous colitis,rhabdomyolysis (muscle breakdown), Stevens-Johnson syndrome, as well as concurrent usage of NSAIDs contributing to the severity of these reactions.
Subsequent to this, on June 25, 2007, the U.S. FDA required the manufacturer to add an additional warning to the package inserts that stated that “Other serious and sometimes fatal events, some due to hypersensitivity, and some due to uncertain etiology, have been reported in patients receiving therapy with quinolones, including ciprofloxacin.”[70] It was not until 2008, (four years later) that the label revisions for ciprofloxacin included any warnings concerning heart problems (prolonged QT Interval / torsades de pointes). Warnings concerning rhabdomyolysis and Stevens-Johnson syndrome are still conspicuously absent from the package inserts as of September 2009.
The serious adverse effects that may occur as a result of ciprofloxacin therapy include irreversible peripheral neuropathy,[71][72] spontaneoustendon rupture and tendonitis,[73][74][75][76] acute liver failure or serious liver injury (hepatitis),[77][78] QTc prolongation/torsades de pointes,[24]toxic epidermal necrolysis (TEN),[79][80][81] and Stevens-Johnson syndrome, severe central nervous system disorders (CNS)[30] andClostridium difficile associated disease (CDAD: pseudomembranous colitis),[82][83] as well as photosensitivity/phototoxicity reactions.
Psychotic reactions and confusional states, acute pancreatitis,[84] bone marrow depression, interstitial nephritis and hemolytic anemia may also occur during ciprofloxacin therapy.[85][86] Additional serious adverse reactions include temporary, as well as permanent, loss of vision,[87][88] irreversible double vision,[89] drug induced psychosis[90][91] and chorea (involuntary muscle movements),[92] impaired color vision, exanthema, abdominal pain, malaise, drug fever, dysaesthesia and eosinophilia.[93][94] Pseudotumor cerebri, commonly known as idiopathic intracranial hypertension (IIH), (also referred to as increased intracranial pressure), has been reported to occur as a serious adverse reaction to ciprofloxacin.[95]
Children and the elderly are at a much greater risk of experiencing such adverse reactions.[96][97] Such reactions may manifest during fluoroquinolone therapy, and long after it had been discontinued.[98]
Serious visual complications have also been reported to occur with ophthalmic fluoroquinolone therapy, which may also occur with ciprofloxacin eye drops, especially corneal perforation, but also evisceration and enucleation. This increased incidents of corneal perforation may be due to fluoroquinolones causing alterations in stromal collagen, leading to a reduction in tectonic strength.[99][100] As noted previously permanent double vision (diplopia) has also been reported.[89] An unusual case of seizures has also been reported with ciprofloxacin ear drops in an elderly patient.[101]
Some groups refer to these adverse events as "fluoroquinolone toxicity". These groups of people claim to have suffered serious long term harm to their health from using fluoroquinolones. This has led to a class action lawsuit by people harmed by the use of fluoroquinolones, as well as legal action by the consumer advocate group Public Citizen.[102] Partly as a result of the efforts of the State of Illinois and Public Citizen, the FDA ordered black box warnings on all fluoroquinolones advising consumers of the possible toxic effects of fluoroquinolones on tendons.[103]
[edit]Interactions
The toxicity of drugs that are metabolised by the cytochrome P450 system is enhanced by concomitant use of some quinolones. Coadministration may dangerously increase coumarin (warfarin) activity; INR should be monitored closely. They may also interact with theGABA A receptor and cause neurological symptoms; this effect is augmented by certain nonsteroidal anti-inflammatory drugs.[104] Quercetin, a flavonol, occasionally used as a dietary supplement, may interact with fluoroquinolones, as quercetin competitively binds to bacterial DNA gyrase. Some foods, such as garlic and apples, contain high levels of quercetin; whether this inhibits or enhances the effect of fluoroquinolones is not entirely clear.[105] Ciprofloxacin can reduce phenytoin plasma levels, which may, in some cases, result in seizures.[106] Ciprofloxacin may interfere with the levels of thyroid medications resulting in hypothyroidism.[107]
On 9 November 2005, the U.S. FDA required the manufacturers to provide additional warnings within the package inserts concerning ciprofloxacin being an inhibitor of human cytochrome P450 1A2 (CYP1A2) mediated metabolism. The new warning stated:
"Coadministration of ciprofloxacin with other drugs primarily metabolized by CYP1A2 results in increased plasma concentrations of these drugs and could lead to clinically significant adverse events of the coadministered drug."[108]
Concurrent administration of ciprofloxacin with magnesium or aluminum antacids, sucralfate or products containing calcium, iron, or zinc (including multivitamins or other dietary supplements) may substantially decrease the absorption of ciprofloxacin, resulting in serum and urine levels considerably lower than desired.[109]
[edit]Significant drug interactions
Ciprofloxacin can alter and be altered by the metabolism and effects of other drugs, resulting in some significant drug-drug interactions that may affect the musculoskeletal, central nervous, renal, and other systems.
Current or past treatment with oral corticosteroids is associated with an increased risk of achilles tendon rupture, especially in elderly patients who are also taking the fluoroquinolones.[110] This is the subject of Black box warnings in FDA and BNF labeling for quinolones.
The Committee on the Safety of Medicines and the FDA warn that central nervous system adverse effects, including seizure risk, may be increased when NSAIDs are combined with quinolones.[24][111] The interaction between quinolones and NSAIDs is important, because it has the potential for considerable CNS toxicity. The mechanism for this interaction is believed to be due to a synergistic increased antagonism of GABA neurotransmission.[65]
Ciprofloxacin's renal clearance may affect other drugs subject to renal clearance or otherwise affecting the kidney. The use of ciprofloxacin concomitantly with cyclosporine has also been associated with transient elevations in serum creatinine. Renal tubular transport ofmethotrexate may be inhibited by concomitant administration of ciprofloxacin, potentially leading to increased plasma levels of methotrexate and risk of methotrexate toxicity. Probenecid interferes with renal tubular secretion of ciprofloxacin and produces an increase in the level of ciprofloxacin in serum.[24]
Some quinolones, including ciprofloxacin, exert an inhibitory effect on the cytochrome P-450 enzyme CYP1A2, thereby reducing clearance, and thus increasing blood levels of tizanidine and methylxanthines (e.g., theophylline and caffeine).[112][113] The quinolones have also been reported to enhance the effects of warfarin or its derivatives.[24] Such interactions can augment the effects of the co-administered drug, including adverse effects. Ciprofloxacin can reduce effects of other drugs; for example, it has been shown to interact with thyroid medications (levothyroxine), resulting in unexplained hypothyroidism.[114] Altered serum levels of phenytoin (increased and decreased) have been reported in patients receiving concomitant ciprofloxacin.[24]
[edit]Overdose
Overdose of ciprofloxacin may result in reversible renal toxicity. Treatment of overdose includes emptying of the stomach via induced vomiting or by gastric lavage. Careful monitoring and supportive treatment, monitoring of renal function and maintaining adequate hydration is recommended by the manufacturer. Administration of magnesium, aluminum, or calcium containing antacids can reduce the absorption of ciprofloxacin. Hemodialysis or peritoneal dialysis removes only less than 10 percent of ciprofloxacin.[109] Ciprofloxacin may be quantitated in plasma or serum to monitor for drug accumulation in patients with hepatic dysfunction or to confirm a diagnosis of poisoning in acute overdose victims.[115]
[edit]Chemistry
Ciprofloxacin is 1-cyclopropyl-6-fluoro-1,4-dihydro-4-oxo-7-(1-piperazinyl)-3-quinolinecarboxylic acid. Its empirical formula is C17H18FN3O3 and its molecular weight is 331.4 g/mol. It is a faintly yellowish to light yellow crystalline substance.[109]
Ciprofloxacin hydrochloride (USP) is the monohydrochloride monohydrate salt of ciprofloxacin. It is a faintly yellowish to light yellow crystalline substance with a molecular weight of 385.8 g/mol. Its empirical formula is C17H18FN3O3HCl•H2O.[109]
[edit]Pharmacokinetics
The effects of 200–400 mg of ciprofloxacin given intravenously are linear; drug accumulation does not occur when administered at 12 hour intervals. Bioavailability is approximately 70-80%, with no significant first pass effect. IV administration produces a similar serum levels as those achieved with administration of 500 mg administered orally. IV administration over 60 minutes given every 8 hours produces similar serum levels of the drug as 750 mg administered orally every 12 hours.[109] Biotransformation is hepatic. The elimination half life is 4 hours.[24]
[edit]History of the black box warnings
See also: Quinolone#Black box warnings
Musculoskeletal disorders attributed to use of quinolone antibiotics were first reported in the medical literature in 1972, as an adverse reaction to nalidixic acid.[116] Rheumatic disease after use of a fluoroquinolone (norfloxacin) was first reported eleven years later.[117] In response to a 1995 letter published in the New England Journal of Medicine, representatives of the U.S. Food and Drug Administration (FDA) stated that the agency would "update the labeling [package insert] for all marketed fluoroquinolones to include a warning about the possibility of tendon rupture."[118]
By August 1996, the FDA had not taken action, and the consumer advocacy group Public Citizen filed a petition with the FDA prompting the agency to act.[119] Two months later, the FDA published an alert in the FDA Medical Bulletin and requested that fluoroquinolone package inserts be amended to include information on this risk.[73]
Nine years later, in 2005, the Illinois Attorney General filed a second petition with the FDA again seeking Black Box Warnings and "Dear Doctor" letters emphasizing the risk of tendon rupture; the FDA responded that it had not yet been able to reach a decision on the matter.[120] In 2006, Public Citizen, supported by the Illinois Attorney General, renewed its demand of ten years prior for Black Box Warnings by filing a third petition requesting such changes be made.[120][121] When the FDA failed to respond to these two petitions as required by law Public Citizen, in January 2008, filed suit to compel the FDA to respond to their 2006 petition.[122][123] On July 7, 2008 the FDA requested that the makers of systemic-use fluoroquinolones add a boxed warning regarding spontaneous tendon ruptures, and to develop a Medication Guide for patients.[124] The package inserts for Ciprofloxacin, Avelox (moxifloxacin), Proquin XR, Factive (gemifloxacin), Floxin (ofloxacin), Noroxin (norfloxacin) and Levaquin (levofloxacin) were amended on September 8, 2008 to include these new warnings.[125] Bayer, which manufactures Cipro, Avelox and Proquin XR, issued a Dear Healthcare Professional letter on October 22 concerning these changes.[126]Ortho-McNeil, the manufacturers of Levaquin, issued a similar letter in November.[127] through the Health Care Notification Network, a registration-only website that distributes drug alerts to licensed healthcare professionals.
Review of the FDA website indicates that the majority of the generic versions of the fluoroquinolones have not been updated to include this Black Box Warning as of September 2009. Additionally there are numerous reports that this information has not been dessiminated to the pharmacist, the name brand products continue to contain the previous labels that are absent of this warning, and the Medication Guide has not been made available to the pharmicist or physician for distribution.
[edit]FDA warning letters
Additionally the manufacturers of ciprofloxacin (Bayer A.G.) received numerous warning letters from the United States Food and Drug Administration regarding false advertising and failure to provide adequate warnings within their promotional materials.[128][129]
[edit]Overprescribing and bacterial resistance
See also: Antibiotic abuse and Antibiotic resistance
Ciprofloxacin is commonly used for urinary tract and intestinal infections (traveler's diarrhea) and was once considered a powerful antibiotic of last resort,[130][131][132] used to treat especially tenacious infections. Not all physicians agreed with this assessment, as evidenced by its wide spread use to treat minor infections as well as non-approved uses. As a result in recent years many bacteria have developed resistance to this drug, leaving it significantly less effective than it would have been otherwise.[133][134]
Resistance to ciprofloxacin and other fluoroquinolones may evolve rapidly, even during a course of treatment. Numerous pathogens, includingStaphylococcus aureus, enterococci, and Streptococcus pyogenes now exhibit resistance worldwide.[135] Widespread veterinary usage of the fluoroquinolones, particularly in Europe, has been implicated.[136]
Fluoroquinolones had become the most commonly prescribed class of antibiotics to adults in 2002.[137] Nearly half (42%) of these prescriptions were for conditions not approved by the FDA, such as acute bronchitis, otitis media, and acute upper respiratory tract infection, according to a study that was supported in part by the Agency for Healthcare Research and Quality.[137][138] Additionally they are commonly prescribed for medical conditions that are not even bacterial to begin with, such as viral infections, or those to which no proven benefit exist.
[edit]Current litigation
Bayer AG A class action had been filed against Bayer AG on behalf of employees of the Brentwood Post Office in Washington, D.C., and workers at the U.S. Capitol, along with employees of American Media, Inc. in Florida and postal workers in general who allege that they have suffered serious adverse effects from taking the antibiotic ciprofloxacin (Cipro) in the aftermath of the anthrax attacks in 2001. The adverse effects included; tendon rupture, seizures, intestinal problems, tendonitis, anxiety, insomnia, muscle aches, depression and meniscus tears. The action alleged that Bayer failed to warn class members of the potential side effects of the drug, thereby violating the Pennsylvania Unfair Trade Practices and Consumer Protection Laws. According to the allegations within the complaint, exposed individuals were not informed of the true safety profile of ciprofloxacin, the high rate of adverse events associated with its use, or the availability of safer and equally effective alternative drugs. The complaint further alleged that, as a result of taking Cipro, many individuals suffered severe and debilitating injuries. The action sought funding for a medical monitoring program and compensatory damages for those workers who have suffered side effects. In 2004, the law firm of Goodell, DeVries, Leech & Dann, LLP were retained as national counsel in this litigation. The class action was defeated and the litigation abandoned by the plaintiffs.[139][140][141] A similar action had been filed in New Jersey that covers New Jersey postal workers. Final disposition of that lawsuit is unknown. Following the addition of the Black Box Warning in 2008, regarding tendon damage, a significant number of product liability law firms began soliciting clients who have suffered a spontaneous tendon rupture following fluoroquinolone therapy.[142][143][144]









I feel ecstatic I found you website and blogs. can-C Free shipping
ReplyDelete